Association of structural changes in the transplanted kidney assessed by magnetic resonance imaging with early graft function
Andrejus Bura1, Antanas Jankauskas2, Justina Karpaviciute1, Marija Ramanauskaite1, Gintare Stonciute-Balniene2, Audra Banisauskaite2, Laura Velickiene2, Ruta Vaiciuniene1.
1Nephrology department, Lithuanian University of Health Sciences, Kaunas, Lithuania; 2Radiology department, Lithuanian University of Health Sciences, Kaunas, Lithuania
Introduction: Kidney transplantation from a deceased donor involves potentially deleterious processes impacting kidney microstructure and function. The magnetic resonance imaging (MRI) and histological evaluation of the transplanted kidney (kTx) have been used to explore associations with graft function and fibrosis. Our study combines kTx biopsies performed after kTx blood supply recovery with MRI conducted 7-10 days post-transplantation, providing an initial understanding of the underlying processes.
Aim: To assess the relationship between structural changes in the kTx, evaluated by MRI and protocol biopsy, and early graft function.
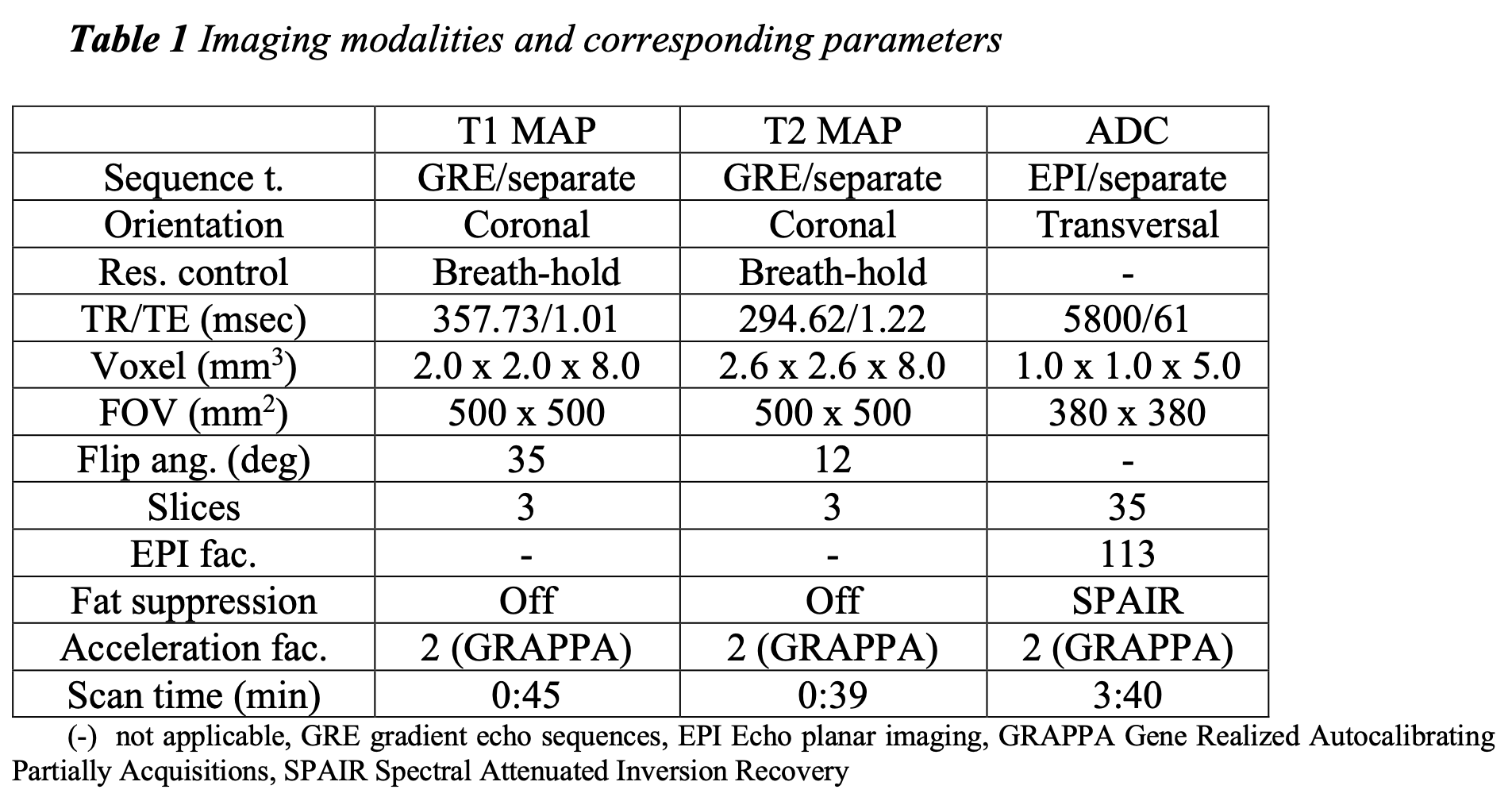
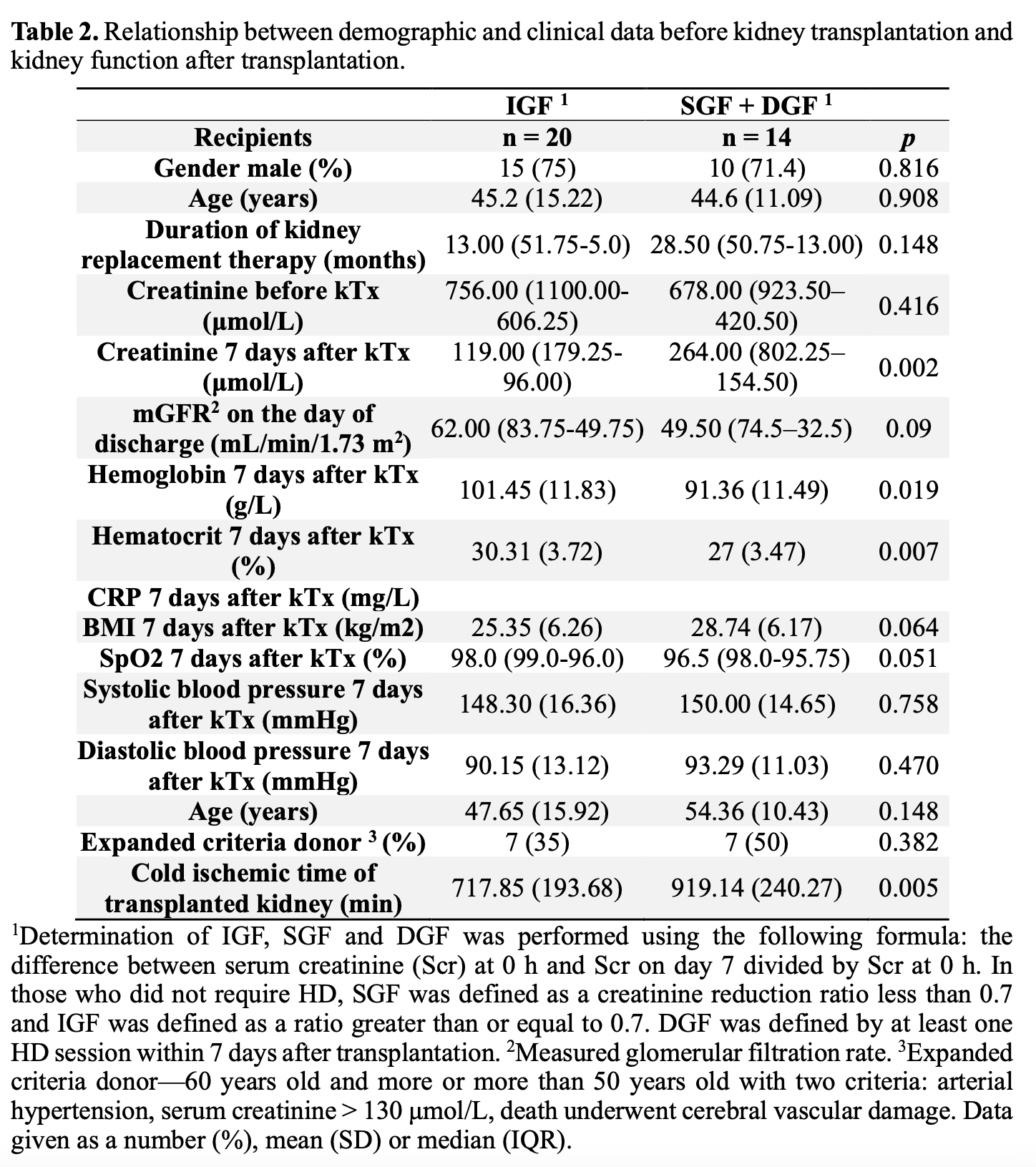
Method: Following approval from the ethics committee, we conducted a prospective study at the Hospital of Lithuanian University of Health Sciences Kaunas Clinics. We performed MRIs of transplanted kidney using a 3T Siemens Skyra scanner (parameters in Table 1) for 34 recipients 7-10 days after successful kTx. Radiologists and a nephrologist scored the MRI images. We employed Parametric Magnetic Resonance Imaging v1.2.31-b for T1, T2 Map, and apparent diffusion coefficient (ADC) for kTx image analysis. Two regions were defined for kTx: cortex and medulla, with the manual placement of regions of interest. The interclass correlation coefficient between investigators was 0.96 for all images. Measurements were averaged across two observers, and mean and standard deviations were calculated. The derived corticomedullary difference (CMD) was also calculated. The kTx biopsy performed during the transplantation was evaluated according to the Banff-2019 criteria. We evaluated early graft function using the classification proposed by Isaac E. Hall and co-authors: immediate, slow, and delayed graft function (IGF, SGF, DGF). Clinical and laboratory data were collected and are presented in Table 2. Statistical analysis was performed using IBM SPSS Statistics version 29.
Results: Recipients were categorized into two groups: IGF (n=20) and SGF/DGF (n=14). We found no differences in T1 and T2 relaxation times, ADC and histological data analysis between IGF and SGF/DGF groups. However, we found a negative correlation between CMD in T1 and the measured glomerular filtration rate (mGFR) on the discharge day (r = -0.383, p = 0.025). Further analysis using univariate linear regression demonstrated a significant negative association between CMD in T1 and mGFR (β coefficient = -0.126, 95% CI [-0.240 to -0.013], p = 0.03). Additionally, CMD in ADC showed a significant positive association with mGFR (β coefficient = 0.095, 95% CI [0.015 - 0.176], p=0.022). Even after adjusting for potentially relevant confounders (such as cold ischemic time), CMD in T1 and ADC remained significant predictors.
Conclusions:
1. Structural differences in MRI and biopsy data were not found between the immediate and deteriorative graft function groups.
2. CMD in T1 and the ADC map showed a significant correlation to mGFR and thereby may serve as potential predictors of early graft function.