
Immune phenotype of interstitial inflammation and tubulitis in T cell-mediated rejection: A study using CODEX multiplexed imaging and machine learning
Angelica Perez-Gutierrez1, Madeleine S Durkee2,3, Junting Ai3, Gabriel Casella2,3, Thao Cao4, Anthony Chang5, Michael S Andrade1, Beatriz Concepcion3, Dustin Shaw6, John J Fung1, Rolf N Barth1, Maryellen L Ginger2, Marcus R Clark3, Anita Chong1.
1Surgery, University of Chicago , Chicago, IL, IL, United States; 2Radiology, University of Chicago , Chicago, IL, IL, United States; 3Medicine, University of Chicago , Chicago, IL, IL, United States; 4Pritzker School of Molecular Engineering, University of Chicago , Chicago, IL, IL, United States; 5Pathology, University of Chicago , Chicago, IL, IL, United States; 6Pritzker School of Medicine, University of Chicago , Chicago, IL, IL, United States
Introduction: Kidney transplantation is the best treatment for end-stage renal disease; however, graft survival is compromised by rejection. T cell-mediated rejection (TCMR) is characterized by the infiltration of immune cells leading to interstitial inflammation and tubulitis. However, the specific characteristics of these infiltrating immune cells are not well defined. A deeper understanding of the composition of the immune infiltrate is crucial for understanding rejection and developing more effective treatments.
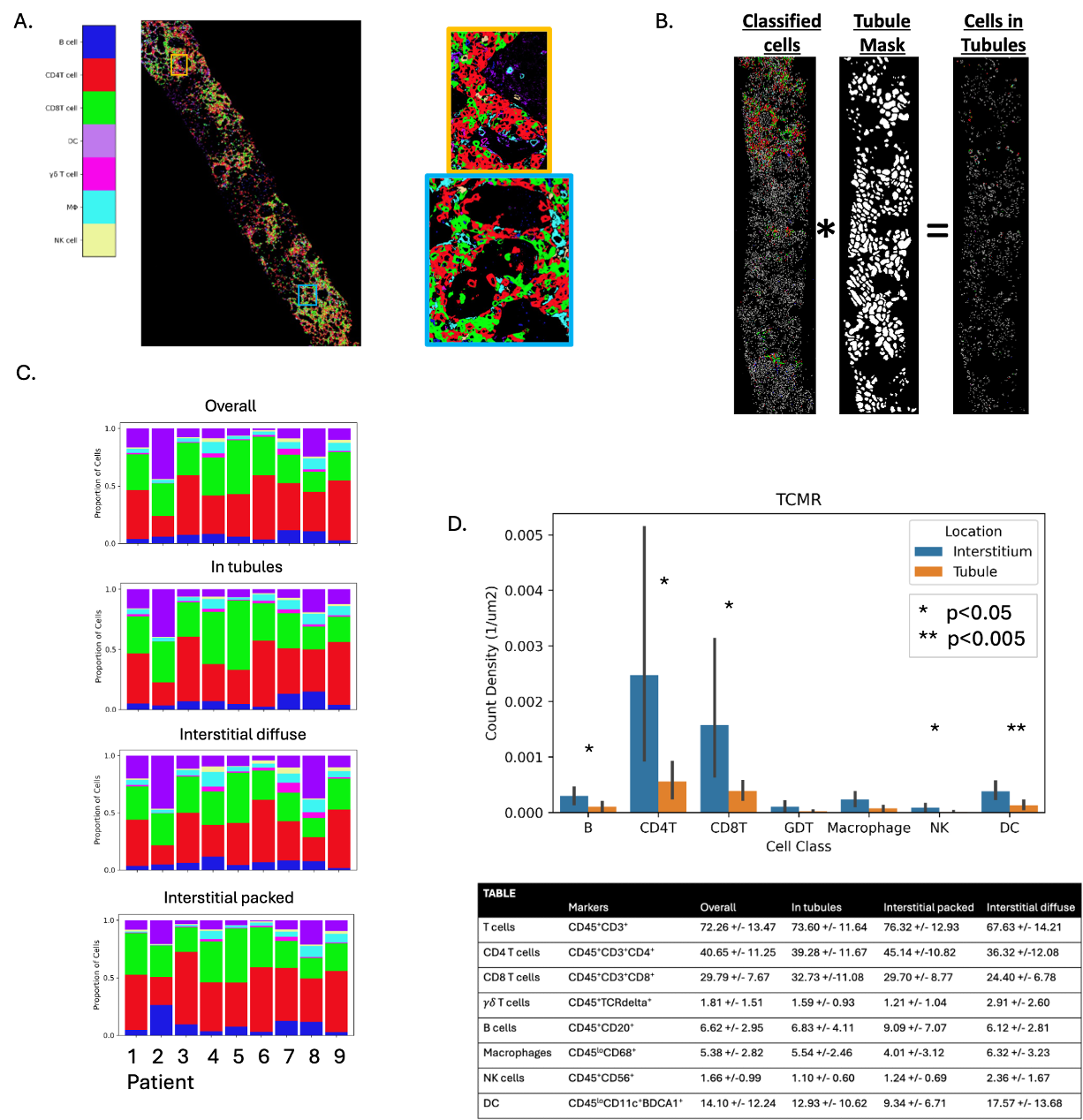
Methods: We conducted co-detection by indexing (CODEX) multiplex imaging on nine graft biopsies from TCMR cases (Banff 1A) using a panel of 44 markers that defined renal cells and CD45+ immune infiltrate. Cells were detected using a fine-tuned Cellpose2.0 model and classified using a spectral angle mapping-based algorithm. We classified CD4+ T cells, CD8+ T cells, gamma delta (γδ) T cells, B cells, macrophages, natural killer (NK) cells, and dendritic cells (DC); all renal cells and remaining immune cells were labeled as ‘unclassified’. Tubules were segmented using a custom Omnipose model. Our analysis focused on defining these specific immune cells in two distinct anatomical compartments: interstitium and tubules.
Results: Overall, CD4+ T cells were the most prevalent immune cells (40.65±11.25) in TCMR kidney biopsies, followed by CD8+ T cells (29.79±7.67), dendritic cells (14.10±12.24), and B cells (6.62±2.95). NK and γδ T cells were present at very low frequencies. The table details the proportions of cells across all compartments. CD4+ (39.28±11.67) and CD8+ (32.73±11.08) T cells were equally prevalent within the tubules. 80-90% of all CD45+ cells were in the interstitium. These cells were categorized as diffuse or densely packed (53.69% of all cells in interstitium). Interstitial inflammation was predominantly composed of T cells, DCs, B cells, and macrophages.
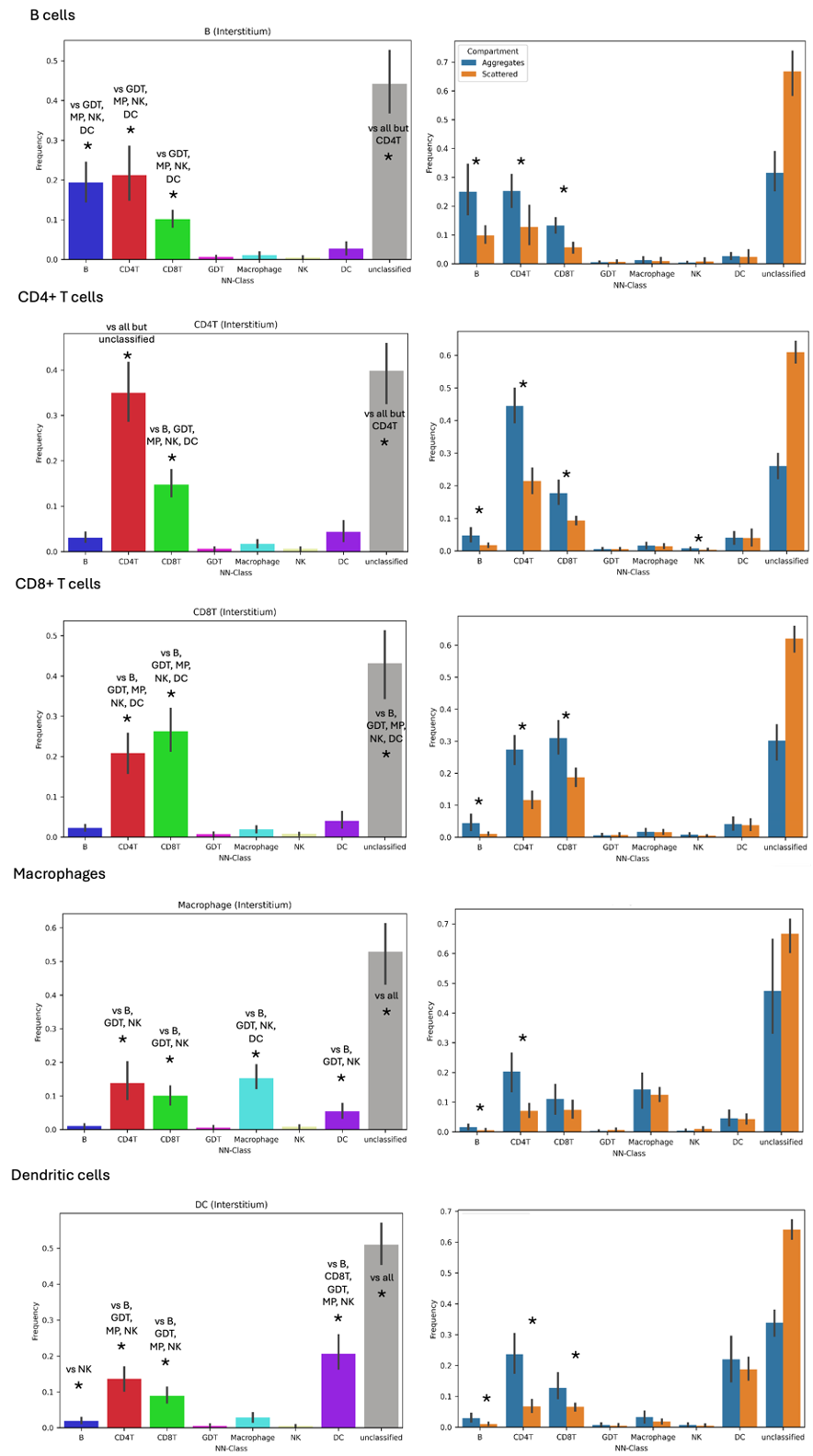
Nearest neighbor analysis of cells in tubules showed that CD4+ T cells were typically closest to themselves, and CD8+ T cells were closest to both CD4+ and CD8+ T cells. Within the interstitium, T cells, B cells and DCs were most likely to be closest to themselves, and to T cells. Within the interstitial compartment, all cell types were more likely to be closest to a B cell or CD4+ T cell in densely packed regions relative to areas of diffuse inflammation. B cells, CD4+ T cells, CD8+ T cells, and DCs were also more likely to be closer to a CD8+ T cell in densely packed areas.
Conclusions: Despite recent transcriptomics analysis focusing on CD8+ T cells as primary mediators of TCMR, the most abundant CD45+ cells in TCMR biopsies are CD4+ and CD8+ T cells, followed by DCs, B cells and macrophages. Future analysis will quantify the likelihood of cognate interactions between T cells and tubules or other MHC II+ T cells. These data will provide insights into the potential interactions driving TCMR.
This study received funding from: 5R01AI148705, UChicago Transplant Institute; Alliance for Lupus Research, 5U19AI082724, 5U19AI110483, 5R01AI152443, T32 GM150375.
[1] T cell mediated rejection
[2] immune phenotype
[3] machine learning
[4] CODEX
