
The clinical utility of follow-up allograft biopsies after early acute TCMR in renal transplantation
Aravind Cherukuri1, Stefan Schaub2, Oriol Bestard3, Georg Bohmig4, Olivier Thaunat5, Maarten Naesens6.
1Thomas E. Starzl Transplantation Institute, University of Pittsburgh, Pittsburgh, PA, United States; 2U of Basel, Basel, Switzerland; 3Vll d'Hebron U Hospital, Barcelona, Spain; 4U of Vienna, Vienna, Austria; 5Hospices Civils de Lyon, Lyon, France; 6U Hospitals Leuven, Leuven, Belgium
Introduction: In kidney transplant patients (KTPs), renal function evaluation by seCr is the current gold standard for monitoring response to anti-rejection therapy. How changes in seCr reflect histological response, and whether follow-up histological evaluation adds prognostic value to clinical assessment by seCr is unknown.
Methods: To address this question, we conducted an observational cohort study of KTPs transplanted between 2013 and 2019 at six centers in Europe and USA (Basel, Barcelona, Vienna, Lyon, Leuven & Pittsburgh) and assessed the relationship between Δ serum creatinine (from nadir level pre-index biopsy (Bx) to 6mos post-treatment), follow-up allograft histology and 7-yr graft survival in KTPs with TCMR diagnosed in the first post-transplant year. Patients at all the centers underwent two protocol Bxs at 3mos and 12mos in addition to for-cause Bx.
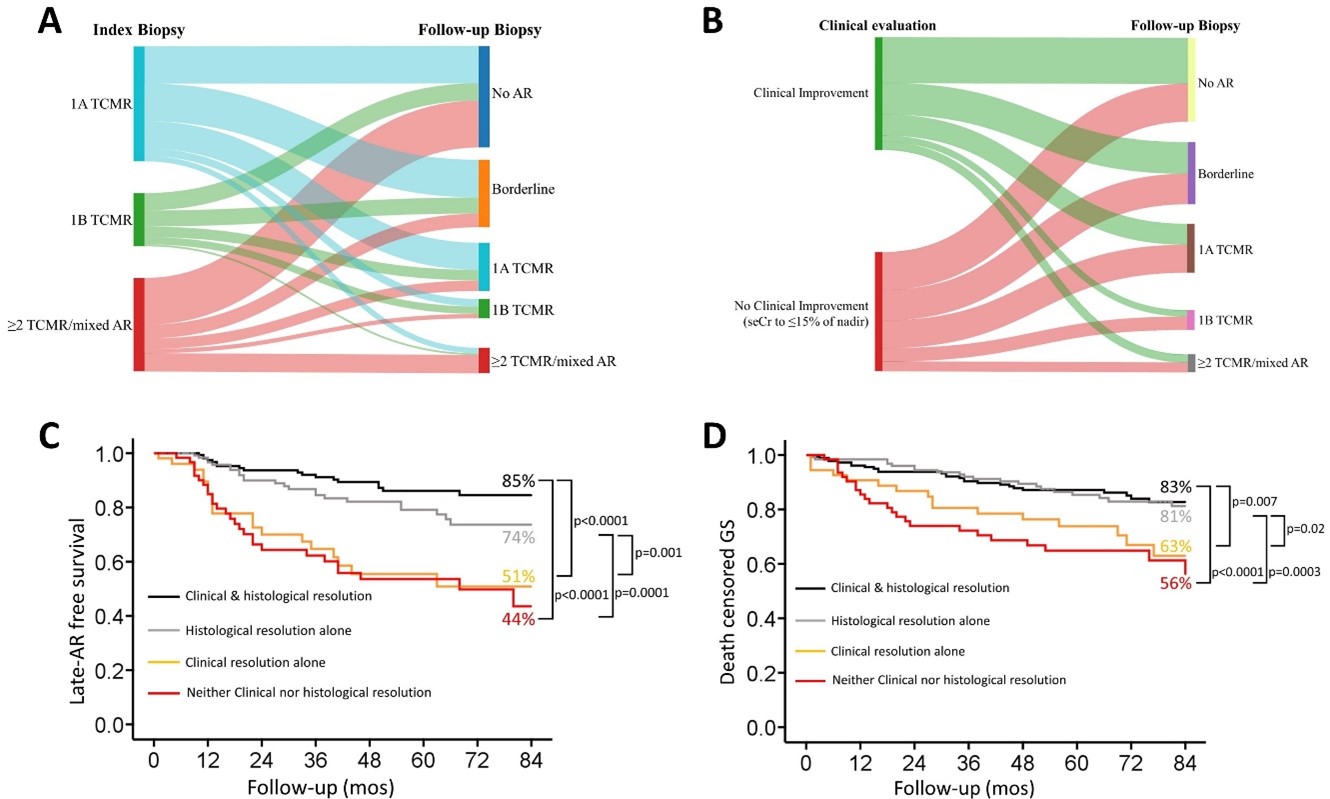
Results: We analyzed 8740 Bxs from 5316 KTPs, of whom 818 (15.4%) had TCMR (47% Banff 1A, 19% 1B, 34% ≥2/mixed TCMR/ABMR) in the 1st post-transplant year. Of these, 73% had at least one follow-up Bx within a year of TCMR diagnosis allowing assessment of histological resolution. Irrespective of TCMR-grade, only 47% of patients exhibited clinical improvement (seCr improvement to ≤15% of nadir) despite anti-rejection therapy. Similarly, only 39% of KTPs had complete histological TCMR-resolution (34% had partial resolution), whereas 27% had persistent TCMR at same/worse grade despite therapy (Fig 1A). Strikingly, TCMR was persistent in 35% of patiets with the mild-1A TCMR, suggesting that histological persistence was not related to rejection severity on index Bx. Only 24% of patients with clinical improvement demonstrated full histological resolution, while 27% had persistent TCMR despite clinical improvement. In contrast, 63% of patients without clinical improvement demonstrated either complete or partial histological resolution, suggesting a clinical-histological mismatch (Fig 1B). Irrespective of index-histological grade and independent of potential confounders, early histological persistence was associated with significantly worse 7-yr-late AR-free survival and 7-yr-death-censored graft survival. Lack of clinical resolution was associated with significantly worse late AR-free survival or graft survival only when there was early histological persistence of TCMR (Figs C&D).
Conclusions: Histological evaluation by follow-up allograft biopsies provides valuable prognostic information after TCMR diagnosis and should be considered in routine clinical practice.
[1] T cell mediated rejection
[2] graft survival
[3] allograft histology
