Effectiveness of the treatment of antibody mediated rejection- a real-world evidence study
Gillian Divard1, Sofia Naser1, Juliette Gueguen6, Marta Crespo4, Ivana Juric3, Brad Astor5, Arnaud Del Bello7, mehdi manaoui2, Alexandre Loupy1, carmen lefaucheur1.
1Paris Institute for Transplantation & Organ Regeneration, Paris, France; 2CHU de Lille, Lille, France; 3Zagreb university hospital , Zagreb, Croatia; 4Hospital Del Mar, Barcelona, Spain; 5University of wisconsin, Madison, WI, United States; 6CHU de Tours, Tours, France; 7CHU de Toulouse, Toulouse, France
Paris Institute for Transplantation & Organ Regeneration.
Background: Antibody-mediated rejection (AMR) is the leading cause of long-term graft failure in kidney transplant recipients (KTR). However, the current standard of care treatment is mainly based on small observational studies. The aim of this study was to provide real world evidence of the effectiveness of AMR treatment in kidney transplant recipients.
Methods: This multicenter prospective cohort study included all patients who presented a first clinical antibody-mediated rejection (active of chronic active) between 2007 and 2020 in four French, two European and one south American centers. AMR cases were reassessed using the latest Banff 2019 classification. All demographic, clinical, biological, immunological, histological and AMR treatments were collected at time of rejection and during the follow-up up to death, graft loss or lost to follow-up. The AMR treatments were separated into several group: no specific treatment, standard of care (SOC), monotherapy or alternative treatment association.
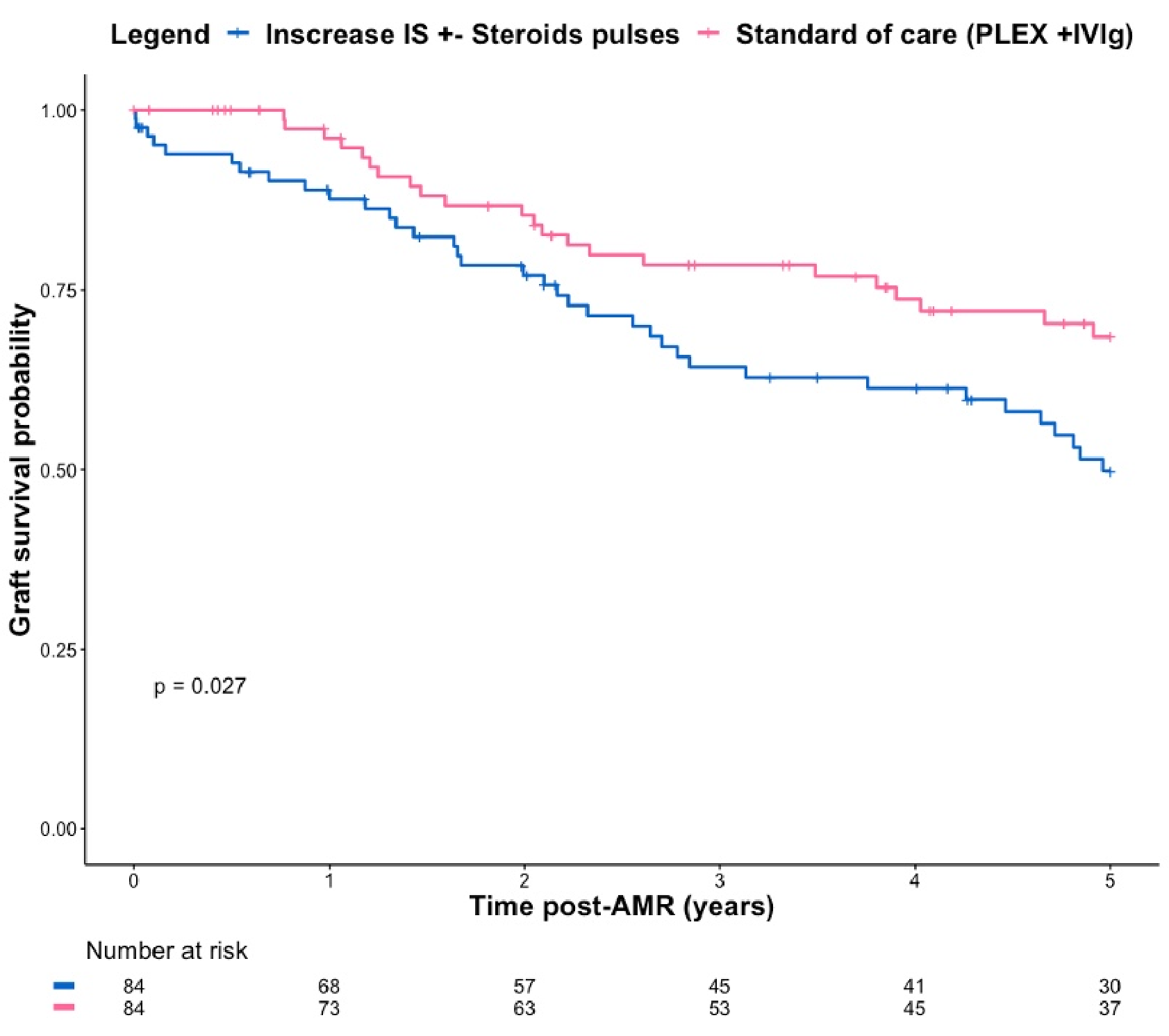
Results: A total of 537 patients were included, with mostly a diagnosis of active AMR (n=383, 71.3%). The AMR occurred in a median time of 16.1 [1.5-58.3] months post-transplantation, mean eGFR was 29.1 (18.4) ml/min/1.73m2, median proteinuria was 0.5 [0.2-1.4] g/g, 386 (76.1%) had positive anti-HLA DSA. In the first 3 months post AMR, 249 (46.4%) patients received a standard of care treatment after AMR, 123 (22.9%) received no specific treatment, 86 (16.0%) received a monotherapy and 79 (14.7%) an alternative treatment association. After a mean follow-up time of 4.1 (3.3) years post AMR, 267 (49.7%) patients experienced graft failure. The absence of specific AMR treatment was highly associated with graft failure (p<0.01) while the association of SOC AMR treatment with graft survival was protective (p=0.04).
 .
.
Conclusions: This study reports the largest cohort of AMR with treated and untreated patients. Antibody-mediated rejection has a severe prognosis that frequently leads to graft failure. This study provides evidence that the standard of care treatment improved transplant outcomes after antibody mediated rejection.
[1] antibody mediated rejection
[2] clinical trial
[3] treatment
[4] outcomes
