Characteristics and outcomes of kidney transplant patients hospitalized for COVID-19 in the United States
Essy Mozaffari1, Aastha Chandak2, Andre C Kalil3, Chidinma Chima-Melton4, Alpesh N Amin5, Mark Berry1, Jason F Okulicz1, Robert L Gottlieb6,7,8.
1Gilead Sciences, Foster City, CA, United States; 2Certara, New York, NY, United States; 3University of Nebraska Medical Center, Omaha, NE, United States; 4University of California, Los Angeles, CA, United States; 5University of California, Irvine, CA, United States; 6Baylor University Medical Center, Dallas, TX, United States; 7Baylor Scott & White The Heart Hospital, Plano, TX, United States; 8Baylor Scott & White Research Institute, Dallas, TX, United States
Background: Immunocompromising conditions and advanced renal dysfunction are individually risk factors for adverse outcomes from COVID-19. We explored the intersection of these risk factors by examining variations in treatment patterns and mortality among hospitalized COVID-19 patients with a history of kidney transplant.
Methods: Patients with a history of kidney transplant (ICD-10-CM: Z94.0) hospitalized in the US for COVID-19 (ICD-10-CM: U07.1) between May 2020-Jan 2023 were identified using the Premier Healthcare Database. Baseline was considered as first two days of hospitalization. We characterized patient demographics, treatment patterns and in-hospital all-cause mortality by chronic kidney disease (CKD) stage as a surrogate for renal allograft dysfunction.
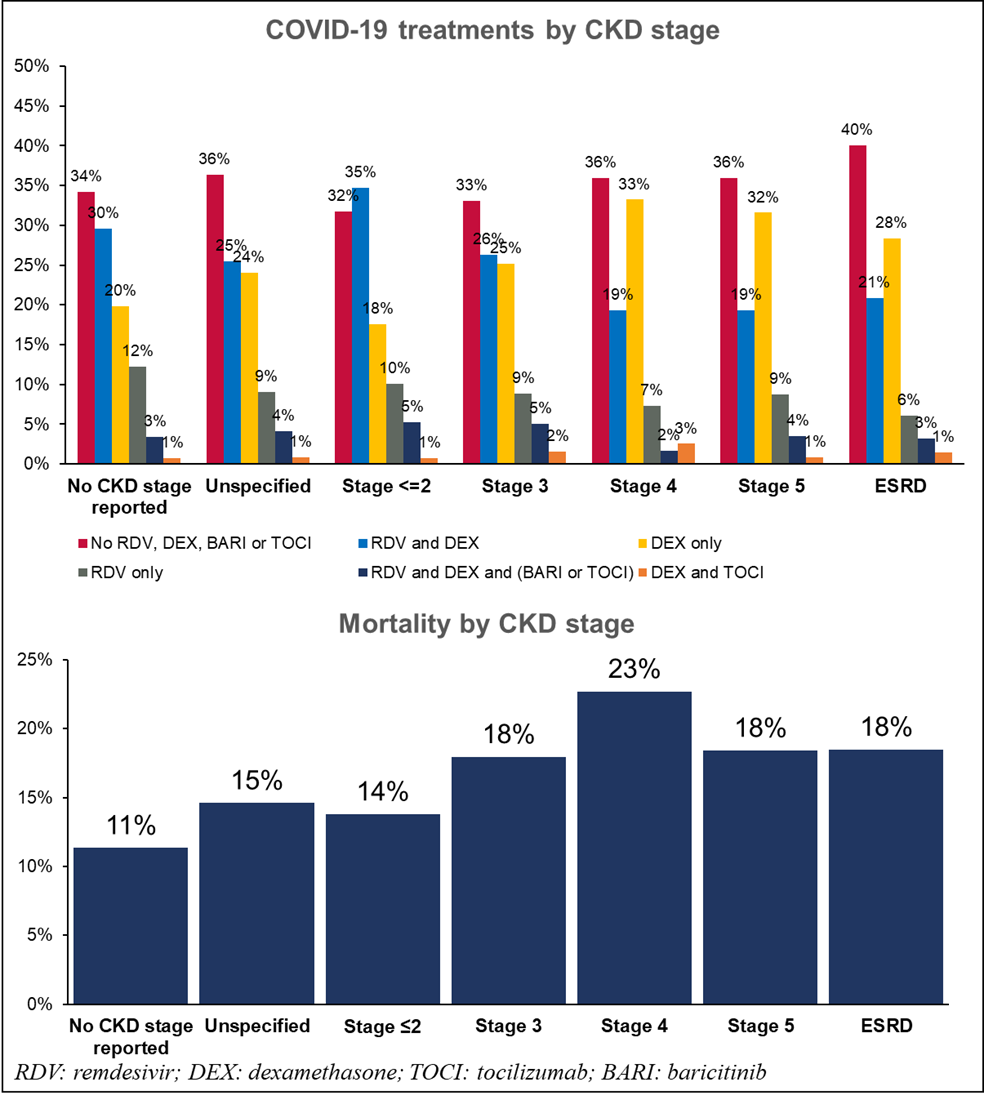
Results: Of the 8,785 patients included in this study from 831 hospitals, 55% were White, 27% Black, 40% female with a median age of 62 years [IQR: 52-70]. Key comorbidities included hypertension (90%) and diabetes (60%). Baseline COVID-19 severity included 68% patients with no supplemental oxygen charges, 17% low-flow supplemental oxygen, 10% high-flow/non-invasive ventilation, and 5% invasive mechanical ventilation/ECMO. Patients were hospitalized for a median of 5 days [IQR: 3-10] with 29% admitted to the ICU and 16% mortality rate. Over the variant periods, patient characteristics remained similar except higher supplemental oxygen requirements, ICU stay and mortality rate in the Delta period as compared to Pre-Delta and Omicron. Despite risk of progression, use of COVID-19 treatments was lower with higher CKD stage, and use of triple therapy with remdesivir+dexamethasone with baricitinib/tocilizumab increased with higher supplemental oxygen requirement (Figure). Mortality increased from 14% for CKD Stage ≤2 to 23% for Stage 4 and 18% for Stage 5 (Figure).
Conclusion: In this study of kidney transplant recipients hospitalized with COVID-19, the lack of any COVID-19 treatment was seen more often as renal function diminished despite a notable increase in overall mortality observed in tandem with compromised renal function. This study sheds light on a persistent therapeutic gap that has affected these patients historically, attributed to factors such as potential drug interactions, past uncertainties regarding the renal clearance of therapeutics, and existing gaps in medical education and awareness. More recent data will be presented at the conference upon acceptance.
[1] Kidney Transplant
[2] COVID-19
[3] Outcomes
