
I am a Professor of Transplant Surgery at the prestigious Post-graduate Institute of Medical Education and Research, Chandigarh India and have been the Head of the Department of Renal Transplant Surgery for the last seven years. I have been trained in Renal Transplant Surgery at this institute and John Hunter Hospital, Newcastle, Australia after receiving primary medical education from Christian Medical College, Ludhiana.
I have been working in the field of transplant surgery for the last 24 years and have been able to contribute to the progress of program not only at my institute but also in the neighbouring region and across the country. My team has helped to initiate transplant activity at many government facilities including medical colleges in various states like Haryana, Himachal Pradesh, Odisha, Jammu etc across India to provide access to kidney transplants to the underprivileged of the society.
The deceased donor transplant at my institute developed from less than 1 donation per year to a robust multiorgan transplant program after my team guided the development of protocols for donor identification, donor consent in triage and donation after circulatory determination of death. Organ donation rates increased from less than 1/year to nearly 40/year leading to 567 deceased donor kidney transplants in addition to other organ transplants over the last 15 years. The living kidney transplant program performs in addition another 250 transplants each year.
I have the privilege of developing the simultaneous kidney and pancreas program in my hospital for Type I diabetic patients presenting with ESRD. The pancreas transplantation was initiated in 2014 and 45 such transplants have been performed which is the highest number in India. I have organized the first national meeting on pancreas transplantation in 2016 and many more such meetings afterward. I was nominated as General Secretary of the newly formed Pancreas Transplant Society of India in 2024, Section Editor (Pancreas) of Indian Journal of Transplantation.
I initiated MCh and fellowship training programs in the field of kidney and pancreas transplantation in India to develop this specialty. I have been a guide to more than 20 transplant surgery trainees who have gone and developed transplant surgery training programs across India and the globe. I am also a guide and co-guide to many PhD Thesis.
I have held important positions in various organizations including the post of Vice President of the Indian Society of Organ Transplantation, founding member of the Pancreas Transplant Society of India, and chair of Organ Transplant Trust which has helped to initiate/promote the deceased organ donation in this region
Over the years, I have received many awards, including the Mentor-Mentee Award 2022 from TTS, Exemplary Performance in Organ Transplantation 2023 in India from the Government of India and helped my institute get awards for four consecutive years (2016-2020) in the field of organ donation
I have initiated normothermic organ perfusion at my institute for the assessment and rejuvenation of kidneys from marginal donors. I received a grant from The Transplantation Society last year to continue our work in this field.
I have also developed the vascular access facility at my institute. The number of vascular access procedures increased from 60/year in 2003 to 1634 vascular access procedures in 2023 to support ESRD patients. The program started routine surveillance of AV access and introduced ultrasound-guided angioplasty for dialysis access to lower cost and ease of procedure for venous stenosis along with other salvage procedures
I have over 150 publications, numerous talks, presentations at scientific meetings and contributed to book chapters. I have authored the Transplant Surgery Manual at my institute. I have been part of the team to develop national guidelines in the Transplant and South East Asian guidelines for Infectious diseases.
Have also developed a Microsoft access based software to maintain a low cost registry of renal transplant patients which hosts data of 4200 transplant patients along with their follow up
Impact of ATG induction therapy on graft and patient survival in living donor kidney transplantation: Insights from the largest single center experience of a public hospital
Ashish Sharma1, Deepesh Kenwar1, Sarbpreet Singh1, Shiva Kumar 1, Devprakash Choudhary1, Sahil Rally1, Jasmine Sethi 2, Parul Gupta3.
1Department of Renal Transplant Surgery , PGIMER , CHANDIGARH , India; 2Department of Nephrology , PGIMER , CHANDIGARH , India; 3Department of Hospital Administration , PGIMER , CHANDIGARH , India
Introduction: Kidney transplantation (KT) is the preferred therapy for individuals with end-stage renal disease (ESRD), offering markedly improved quality of life and survival benefits beyond the constraints of dialysis. While induction therapy with a biologic agent is recommended for kidney transplantation, limiting its usage to patients at high risk for acute rejection has also been proposed to lower costs in appropriate situations per KDOQI guidelines. The long-term impact of this strategy in living-related donor kidney transplantation, particularly in terms of long-term graft and patient survival, remains uncertain. This study represents the most extensive single-center experience to date, evaluating the impact of ATG induction versus no induction on outcomes such as graft survival, patient survival, and allograft rejection rates in the context of living donor kidney transplantation.
Methods: This retrospective single-center study included living donor kidney transplantation (LDKT) performed between September 2008 and December 2022. The study center implemented a low-dose ATG induction protocol, administering 1 mg/kg/day for three consecutive days in cases of LDKT at high-risk profile recipients (such as a history of sensitization, prior transplantation, or mismatched donor-recipient HLA). Conversely, no ATG induction therapy was employed for related LDKT where the recipient has a low-risk profile (characterized by the absence of sensitization and a donor-recipient HLA match greater than 3 out of 6).
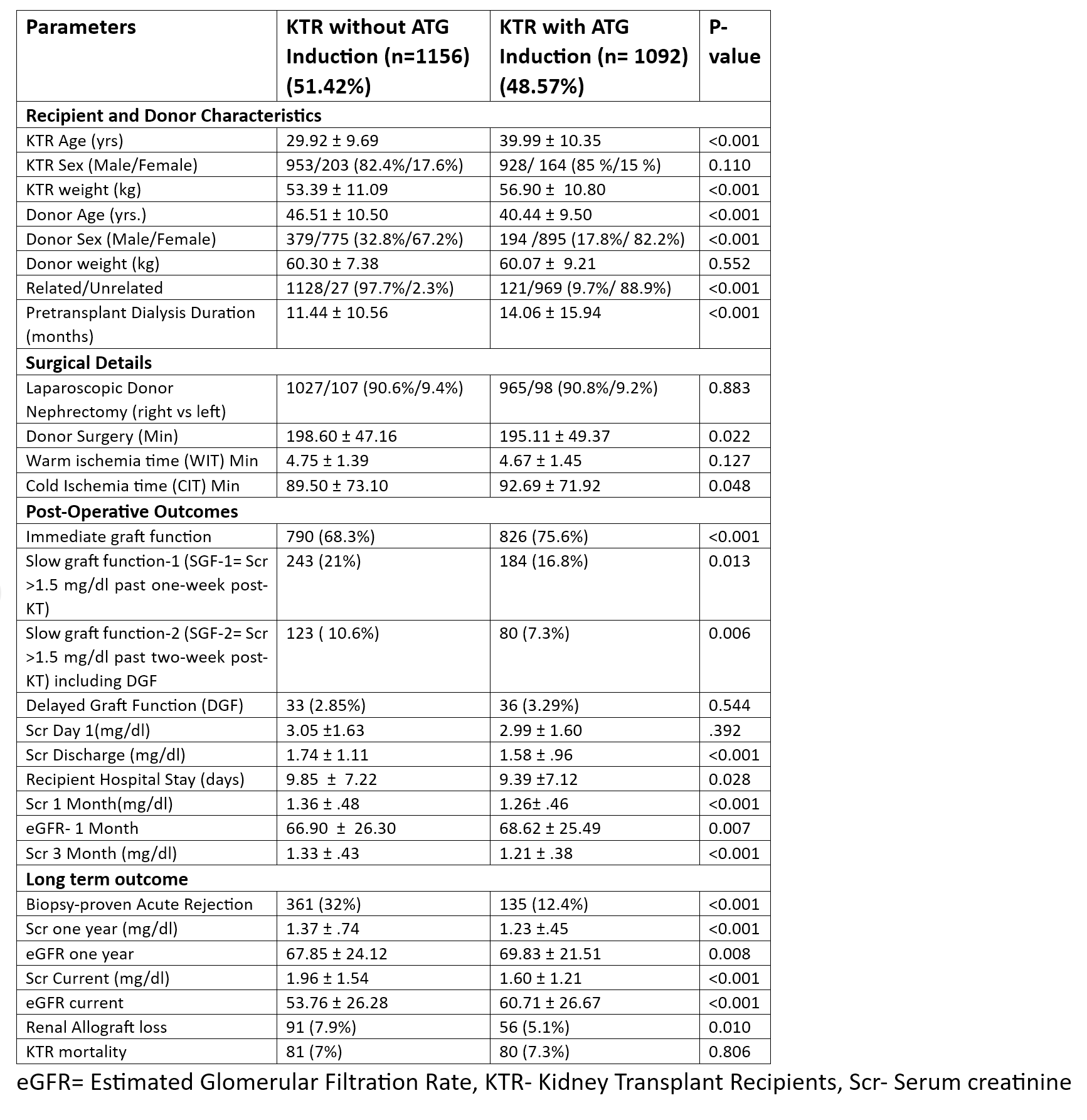
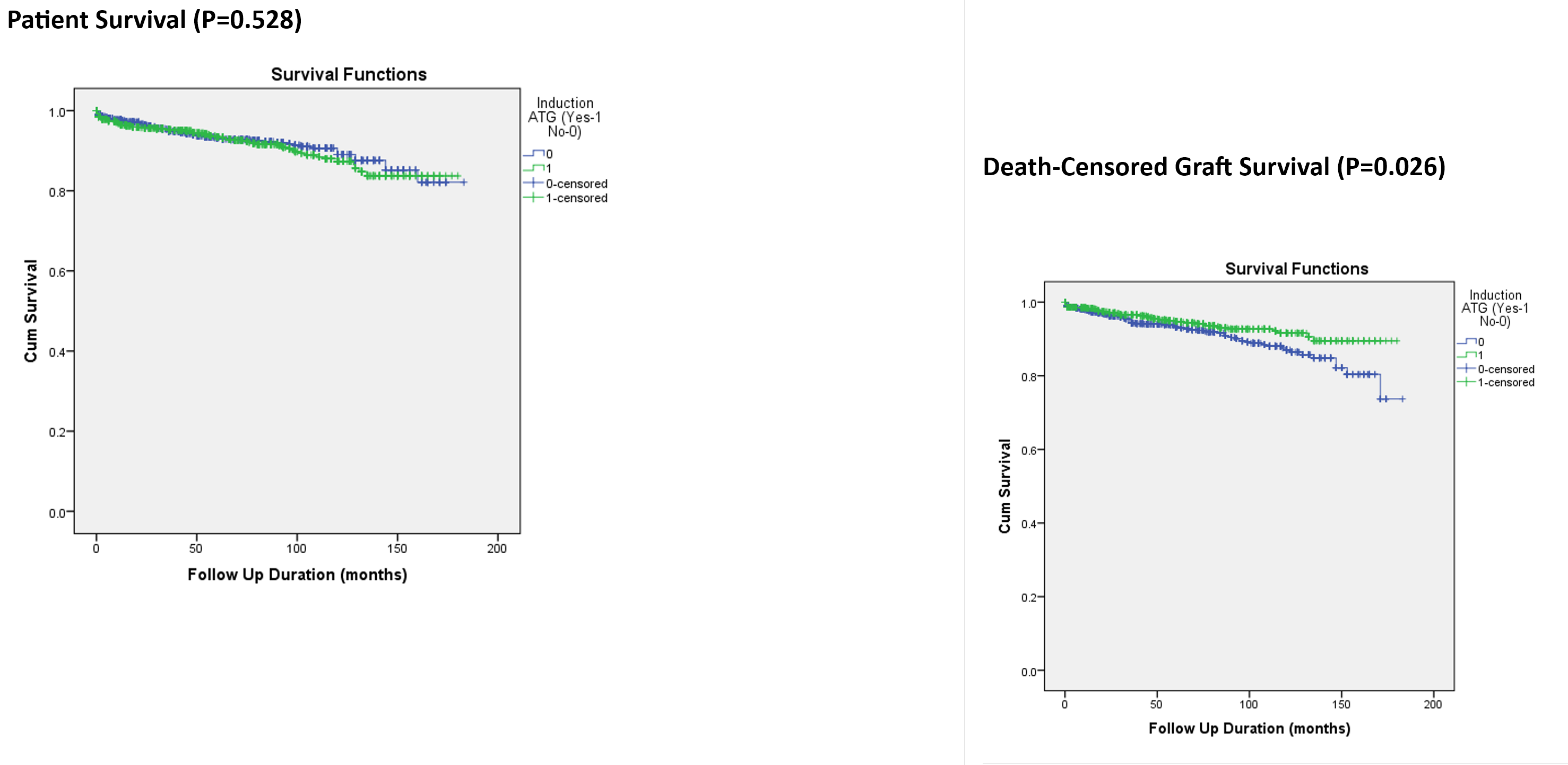
Results: In the analysis of 2,248 LDKT, 48.57% of the kidney transplant recipients (KTRs) received ATG induction. Despite the ATG induction group featuring notably older demographics of KTRs, a higher percentage of unrelated donors, and a more extended period of pre-transplant dialysis, the short-term and long-term outcomes for allograft function and graft survival were significantly better than those without induction. Moreover, the incidence of allograft rejection was substantially reduced in the ATG induction group (Table). Nonetheless, patient survival rates were comparable across both groups throughout the mean follow-up period of 61.86±44.91 months (Figure).
Conclusion: ATG induction therapy significantly enhanced the short-term and long-term allograft function, reduced acute rejection rates, and improved allograft survival in LDKT. Avoiding induction therapy in low-risk situations to reduce costs might not be a good strategy in the long term.
We sincerely thank the Transplant Coordinator team of PGIMER for their valuable insights and contributions to this work.
[1] ATG Induction
[2] Living Donor Kidney Transplantation
[3] Biopsy Proven Acute Rejection
[4] Graft Survival
[5] Patient Survival
