Outcomes of high immunological risk kidney transplantation in an Asian tertiary academic transplant centre
Shilpa Vijayasrinivasan1, Quan Yao Ho2,3, Shan-Yeu Carolyn Tien2,3, Xin Lin Joey Kay3, Jenny Leong2,3, Ian Tatt Liew2,3, Sobhana Thangaraju2,3, Terence Kee2,3.
1Internal Medicine, Singapore General Hospital, Singapore, Singapore; 2Renal Medicine, Singapore General Hospital, Singapore, Singapore; 3SingHealth Duke-NUS Transplant Centre, SingHealth, Singapore, Singapore
Introduction: While high immunological risk kidney transplants (KT) have been associated with poorer outcomes, outcomes in Asian transplant centres are less well established. This study aims to investigate the outcomes of KTs stratified by immunologic risk conducted over a 10-year period at an Asian tertiary academic transplant centre.
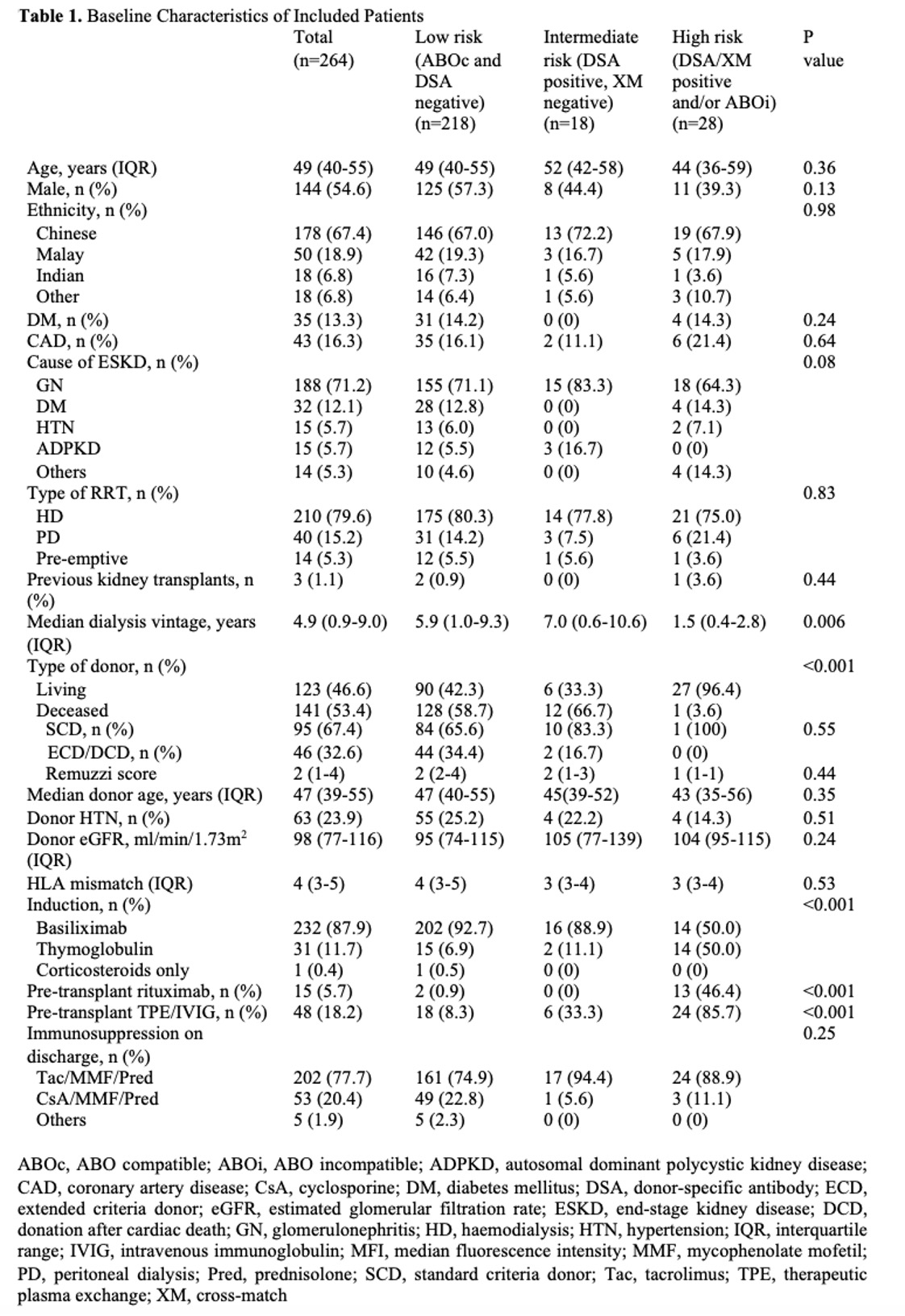
Method: A retrospective chart review of adult KTs performed between January 2012 to May 2021 was conducted. High immunological risk was defined as KTs that were ABO incompatible or complement-dependent cytotoxicity (CDCXM) or flow cross-match (FXM) positive with donor-specific antibodies (DSA), intermediate risk as those who had immunodominant DSA of median fluorescence intensity (MFI) ≥ 1500 but were CDCXM and FXM negative, and low risk as those who were ABO compatible and DSA negative.
Results: A total of 264 patients were included, including 141 deceased donor kidney transplants (DDKT) and 123 living donor kidney transplants (LDKT) with a median follow-up of 6.1 years (interquartile range (IQR) 4.3-9.2). Recipients of high immunological risk KTs had significantly shorter dialysis vintage, and were more likely to receive LDKTs and pre-transplant desensitisation with more intense induction immunosuppression.
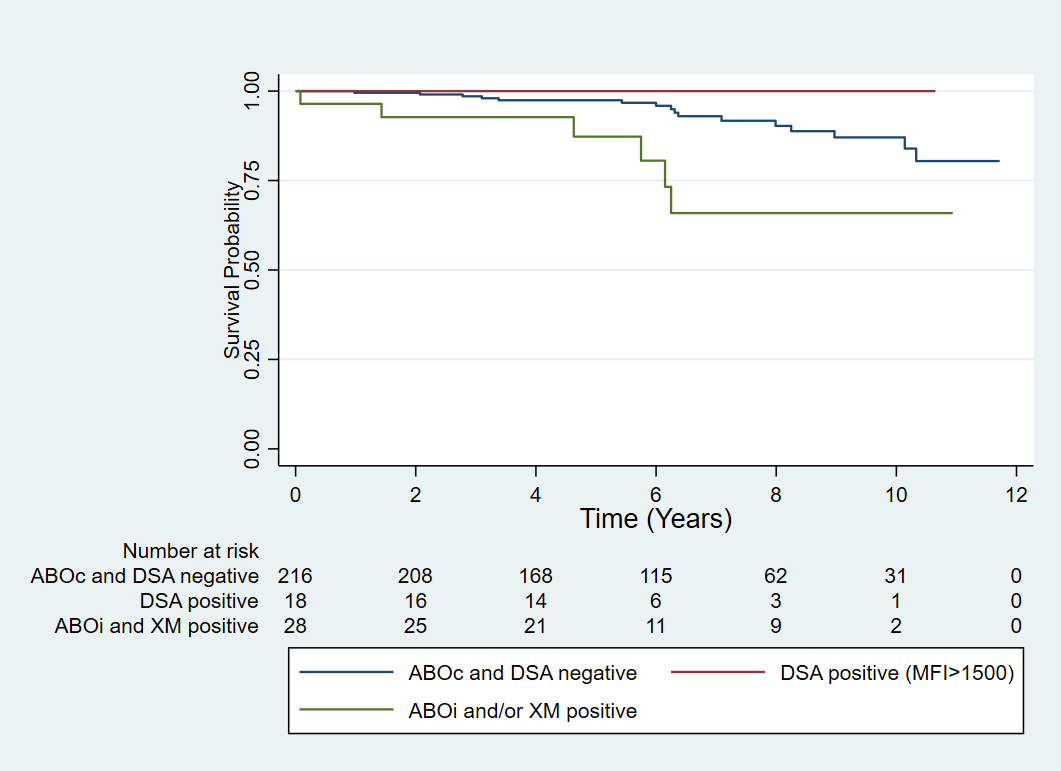
Overall patient survival, graft survival, and graft function at 1 year and 5 years did not differ between the immunological risk groups. However, high immunological risk transplants were associated with increased death-censored graft loss (hazard ratio (HR) 3.31, 95% confidence interval (CI) 1.29-8.50 p=0.01, Figure 1). The association was not significant after adjustment for transplant type, induction therapy, and desensitisation e.g. with plasmapheresis and/or intravenous immunoglobulin and rituximab administration (adjusted HR 0.81 95% CI 0.18-3.58, p=0.78) and on sensitivity analysis by only including LDKTs (HR 2.62, 95% CI 0.93-7.38, p=0.07).
Intermediate-risk KTs were associated with a shorter time to rejection when compared to the low immunological risk KTs (HR 2.39 95% CI 1.14–5.01 p=0.02). This remained significant after adjustment for type of transplant, induction therapy, desensitisation, and rituximab administration. The highest MFI of overall (HR 1.13 per 1000 increase in MFI, 95% CI 1.06-1.21, p<0.0001) and class II (HR 1.12, 95% CI 1.04-1.21, p=0.002) but not class I DSAs (HR 1.13, 95% CI 0.99-1.29, p=0.07) present were associated with rejection. Overall graft and death-censored graft survival did not differ based on the level of MFI of the immunodominant DSAs present.
Conclusion: Higher immunological risk KTs may have poorer graft outcomes, but the risk may be mitigated with appropriate immunosuppression. Higher levels of DSAs were associated with increased rejection but were not associated with poorer graft survival.
[1] High immunological risk
[2] ABO incompatible
[3] Graft survival
[4] Graft rejection
