
Dynamic release of kidney-derived urinary extracellular vesicles: potential biomarkers for acute rejection in kidney transplantation
Liang Wu1,2, Carla C. Baan2, Derek Reijerkerk2, Daan Nieboer3, Thierry P. P. van den Bosch4, Dennis A. Hesselink2, Karin Boer2.
1Department of Nephrology, The First Affiliated Hospital of Shaoyang University, Shaoyang, People's Republic of China; 2Division of Nephrology and Transplantation, Department of Internal Medicine, Erasmus MC Transplant Institute, University Medical Center Rotterdam, Rotterdam, Netherlands; 3Department of Public Health, Erasmus University Medical Centre, Rotterdam, Netherlands; 4Department of Pathology, Erasmus University Medical Centre, Rotterdam, Netherlands
Introduction: Diagnosing acute rejection (AR) after kidney transplantation relies on an invasive kidney biopsy. Novel, preferably non-invasive, markers are needed to indicate AR. Kidney-derived urinary extracellular vesicles (kd-uEVs) hold promise as candidate markers, but a comprehensive understanding of their release after transplantation is lacking. This study aims to elucidate kd-uEV dynamics post-transplant and their potential as biomarkers to distinguish AR from another common allograft complication, acute tubular necrosis (ATN).
Method: In the discovery cohort, urine was collected from donor-recipient pairs (n = 73) pre-transplant and from the recipients on day 3 (D3), day 7 (D7), day 180 (D180), and before a for-cause biopsy post-transplant. Urine from recipients (n=30) with biopsies within two weeks post-transplant served as validation cohort. Urine was centrifuged to remove cells and then stained with the uEV-marker CD63 combined with a kidney-specific marker, aquaporin 2 (AQP2; collecting duct), or podocalyxin (PODXL; podocyte). Kd-uEVs were quantified using imaging flow cytometry. Urine dilution was corrected by calculating kd-uEV percentages in the total CD63+ uEVs.
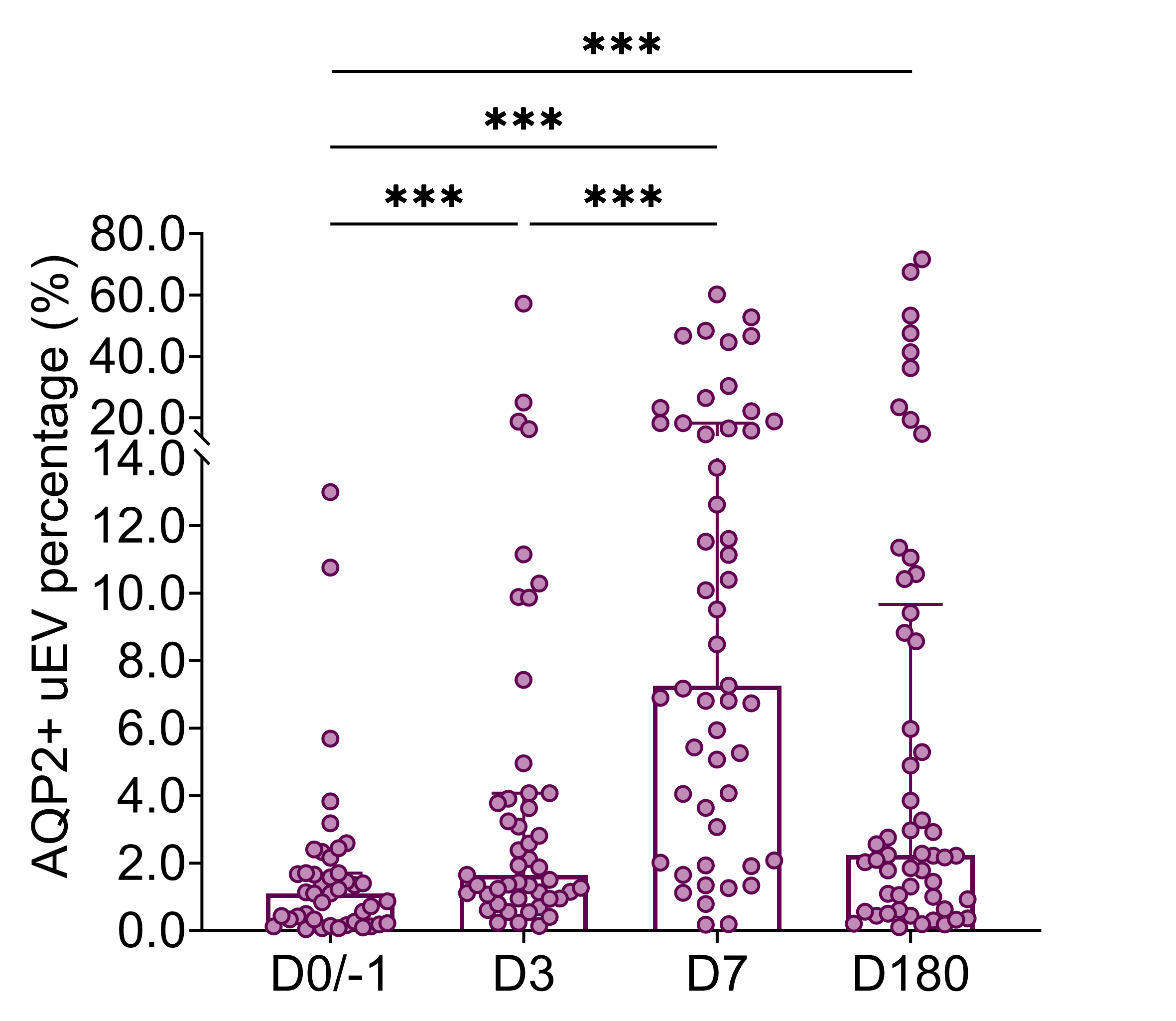
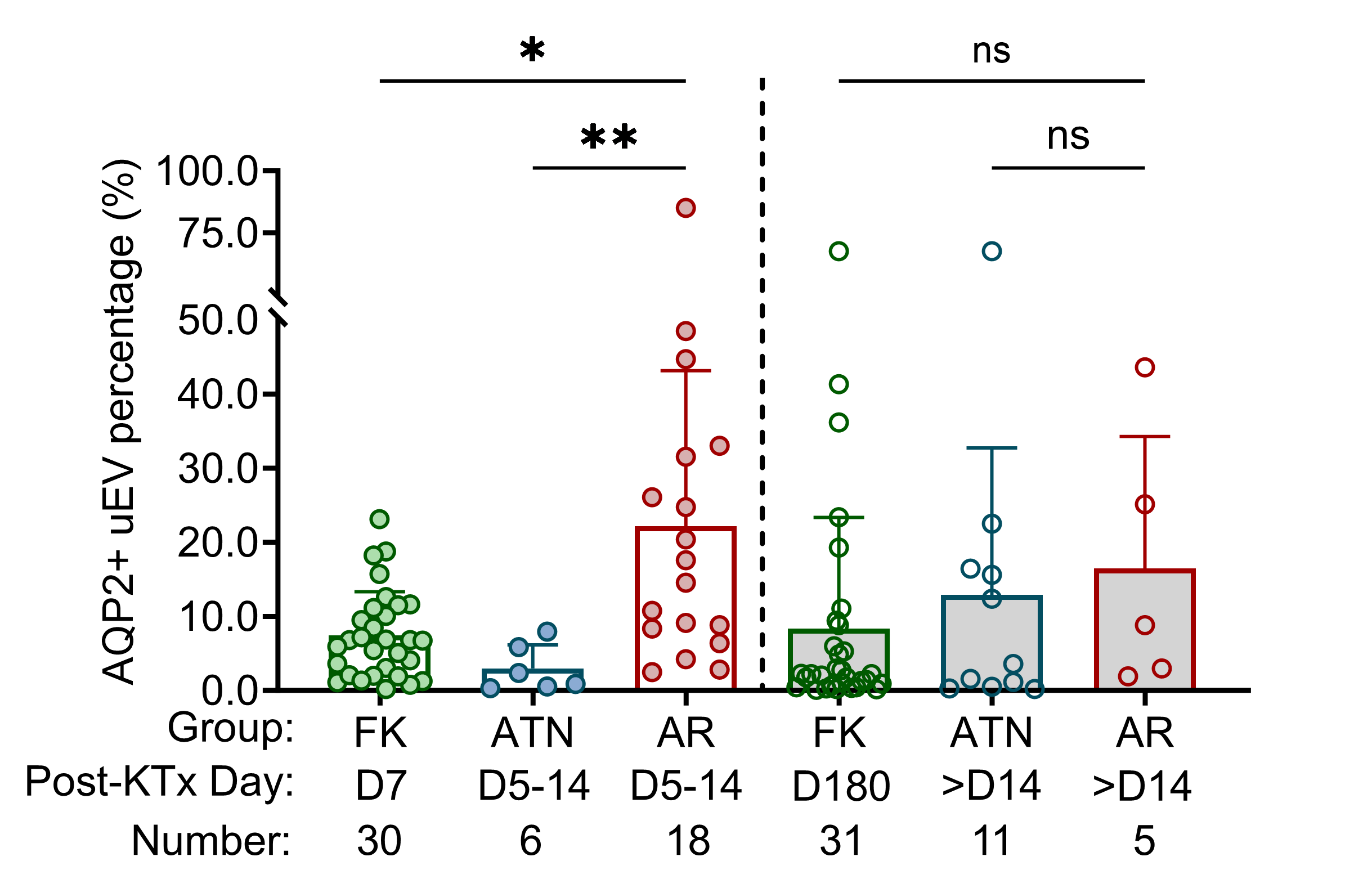
Results: In the discovery cohort, of the CD63+ uEVs from donor urine, 4.2 [0.9 – 11.9]% were AQP2+, and 6.4 [1.5 – 10.7]% were PODXL+. Compared with donors, pre-transplant recipients displayed minimal levels, with 1.1 [0.2 – 1.7]% (p < 0.001; AQP2+) and 1.5 [1.0 – 3.1]% (p < 0.001; PODXL+). These recipient levels remained minimal on D3 but increased on D7 to 7.3 [3.1 – 18.2]% (p < 0.001; AQP2+; Figure 1) and 10.0 [3.2 – 16.3]% (p < 0.001; PODXL+) which persisted until D180. In the discovery cohort, 78% of AR cases occurred in the first two weeks post-transplant. During this period, AR showed a significantly higher level of AQP2+ uEV (16.1 [7.9 – 31.9]%) than the ATN group (1.6 [0.5 – 6.4]%; p = 0.006; Figure 2). Similarly, PODXL+ uEV were also higher in the AR, 13.4 [6.6 – 27.4]%, than the ATN, 3.1 [0.6 – 7.0]% (p = 0.027). The receiver operating characteristic (ROC) analysis demonstrated a 0.934 area under the curve (AUC) for AQP2+ uEV (p = 0.002), 0.868 for PODXL+ uEV (p = 0.008), and 0.925 for the combination (p = 0.002) to distinguish AR from ATN in the first 2 weeks after transplantation. In the validation cohort, still, AQP2+ uEV was observed with an increase in the same period of AR (14.3 [7.1 – 20.4]%) than the ATN (3.3 [1.5 – 5.5]%; p < 0.001). In parallel, PODXL+ uEV was elevated in the AR (9.4 [6.6 – 19.3]%) compared to the ATN (2.9 [4.7 – 10.8]%; p = 0.02).
Conclusion: Post-transplant, AQP2+ uEV release initiates more from D7 than from D3 onwards. For patients with a for-cause biopsy within the initial two weeks after transplantation, increased kd-uEV release indicates AR. These findings underscore the promising potential of kd-uEVs as non-invasive biomarkers for identifying AR early after kidney transplantation.
We acknowledge Weicheng Xu (Erasmus MC Transplant Institute, University Medical Center Rotterdam, Rotterdam, the Netherlands) for the support of IFCM experiments and the sponsorship from the China Scholarship Council (grant number 202008430154). All figures created on BioRender.com were provided with copyright licenses.
[1] Graft Rejection
[2] Kidney Transplantation
[3] Extracellular Vesicles
[4] Biomarker
[5] Acute Tubular Necrosis
[6] Human Urine
