The experience of 1100 cases of hand assisted laparoscopic donor nephrectomy for living donor kidney transplantation
Takahisa Hiramitsu1, Tomoki Himeno1, Yuki Hasegawa1, Kenta Futamura1, Manabu Okada1, Toshihiro Ichimori1, Shunji Narumi1, Yoshihiko Watarai1.
1Transplant and Endocrine Surgery, Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital, Nagoya, Japan
Background: Due to the extreme shortage of the cadaveric donors for kidney transplantation, the number of living donor kidney transplantation (LDKT) is increasing. To lessen the burden of the living kidney donors (LKDs), endoscopic donor nephrectomy is widely performed. The safety of LKDs and graft quality should be secured for the successful LDKT. We investigated the impact of right and left hand assisted laparoscopic donor nephrectomies (HALDNs) on the LKDs.
Methods: Between January 2008 and December 2020, a total of 1157 HALDNs including 81 right and 1076 left HALDNs was performed at our hospital. To compare the safty between both HALDNs, the operative outcomes including operative duration, blood loss, warm ischemia time, adverse events, postoperative estimated glomerular filtration rates (eGFRs), and mortality of LKDs were investigated. To compare the graft quality between both HALDNs, postoperative eGFRs and graft survival of recipients were investigated.
Results: Significant difference was not identified in the operative duration, blood loss, adverse events, postoperative eGFR of LKDs at any time points after operation and mortality (P=0.243), except for the significantly shorter warm ischemia time in right HALDN (P<0.001).
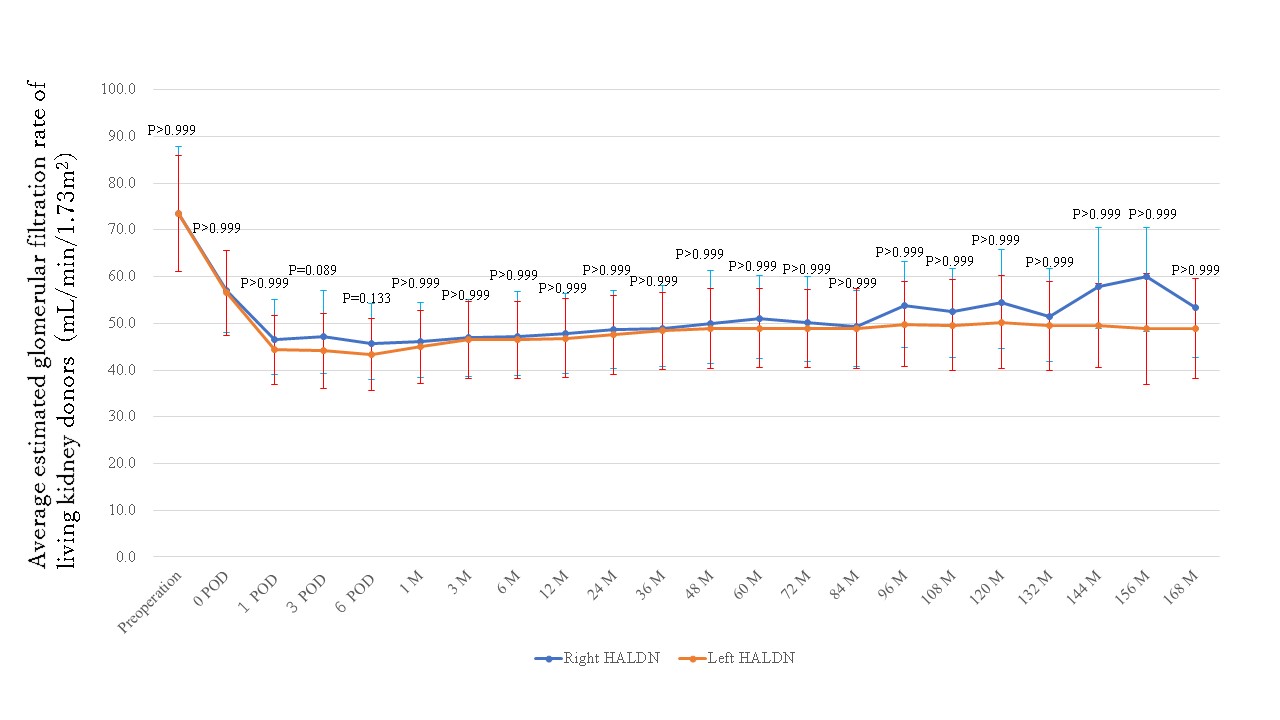
Perioperative death and end-stage renal disease were not identified in both HALDNs. Postoperative eGFR of recipients were similar at any time points after operation.
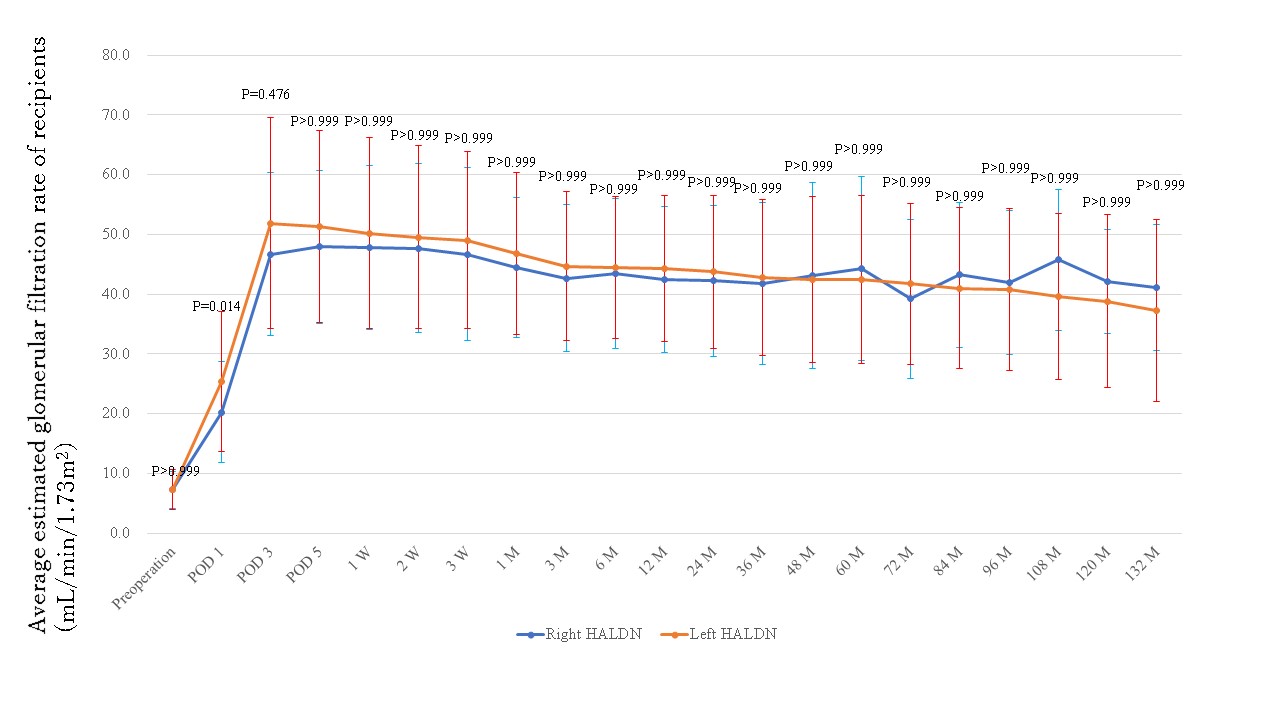
The graft survival rates were similar in both HALDNs (P=0.981).
Conclusion: The safety and graft quality were similar in right and left HALDNs.
[1] living donor kidney transplantation
[2] donor nephrectomy
[3] mortality
[4] eGFR
