Successful long-term somatic support of brain-dead human decedent in pre-clinical xenotransplantation study
Jeffrey Stern1, Imad Aljabban1, Jacqueline I. Kim1, Ian Jaffe1, Shivani Bisen1, Karen Khalil1, Elaina Weldon1, Adam Griesemer1, Robert A. Montgomery1, Phil Sommer1.
1Transplant Institute , NYU Langone Health, New York, NY, United States
NYU Xenotransplant Research Group .
Introduction: We have made significant strides in xenotransplantation over the past few decades using pre-clinical non-human primate (NHP) models. This has culminated in two recent pig-to-human heart xenotransplants. However, despite favorable NHP data, both recipients demonstrated limited survival. This calls into question whether NHP studies can be safely translated to human subjects. Use of human brain-dead decedents (BDD) in xenotransplant research may potentially bridge the gap between NHP studies and clinical trials. However, there remains concern over stability of BDD over extended periods of time. Here, we aimed to investigate if prolonged somatic support of BDD during xenotransplantation study was possible.
Methods: Potential human xenograft recipients were declared brain dead using standard clinical criteria. Once all prospects for organ donation were exhausted and eligibility determined, consent from the family was obtained. The BDD was transferred to New York University (NYU) for stabilization. Bilateral nephrectomies were performed, and an alpha-Gal knockout pig kidney was transplanted into the left extraperitoneal space. Post-operatively the BDD was managed in the intensive care unit (ICU) for two months where routine hemodynamic monitoring was performed. Thyroid hormone, vasopressin, glucocorticoids, and mineralocorticoids were exogenously repleted.
Results: The decedent had labile blood pressure, with mean arterial pressure (MAP) ranging from 47-140 mmHg (Figure 1). Blood pressure (BP) was stabilized using norepinephrine, phenylephrine, vasopressin (average requirements 0.062 mcg/kg/min norepinephrine equivalents), and nicardipine. Despite high BP variability, heart rate always remained within 55-99 bpm (IQR 67-75). Thyroid hormone was replaced with levothyroxine, titrated over several weeks from 360 mcg/day IV to 100 mcg/day oral. Left ventricular ejection fraction remained 65-75% throughout the two months. The decedent was maintained on >10 mg prednisone equivalents and 200 mcg fludrocortisone daily. Nutritional support was provided enterally via jejunostomy tube. Insulin supplementation was provided via continuous infusion. The decedent had a tracheostomy in place and was maintained on pressure control ventilation with daily lung recruitment maneuvers and weekly bronchoscopies. Standard ICU skin care bundles were administered and effective in preventing skin breakdown.
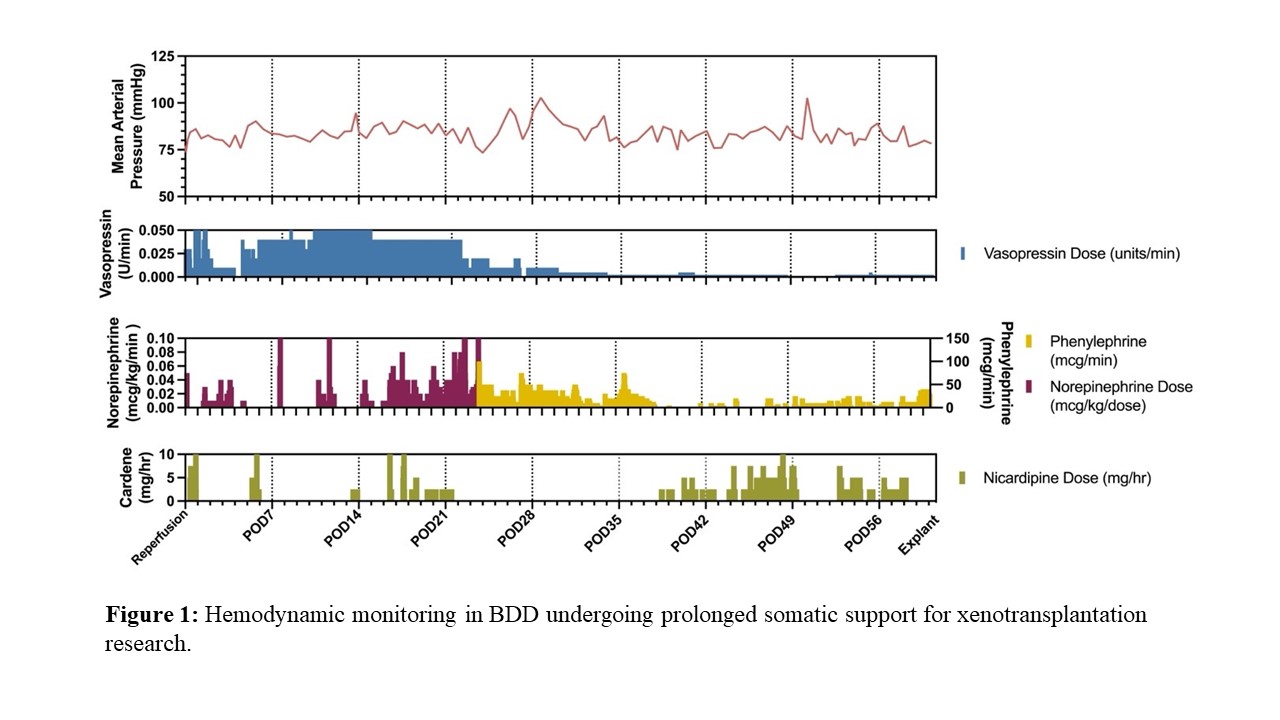
Conclusion: Successful somatic support of BDD over two months was achieved. Decedents appear to have a central vasoplegia responsive to vasopressors, with concomitant vagotomy-like restricted chronotropy. Replacement of hypothalamus-driven hormones is necessary. Nutritional management can be successful with tube feeding and insulin replacement.
Funding for this study was provided by United Therapeutics Corporation.
[1] Xenotransplantation
[2] Somatic Support
[3] Critical Care Medicine
