The world’s first combined face and whole-eye transplant: Technical aspects, surgical underpinnings, and 1-year outcomes
Bruce E. Gelb2, Alay R. Shah1, Sachin R. Chinta1, David L. Tran1, Daniel J. Ceradini1, Eduardo D. Rodriguez1.
1Hansjörg Wyss Department of Plastic Surgery, New York University Langone Health , New York, NY, United States; 2Department of Surgery, New York University Langone Health, New York, NY, United States
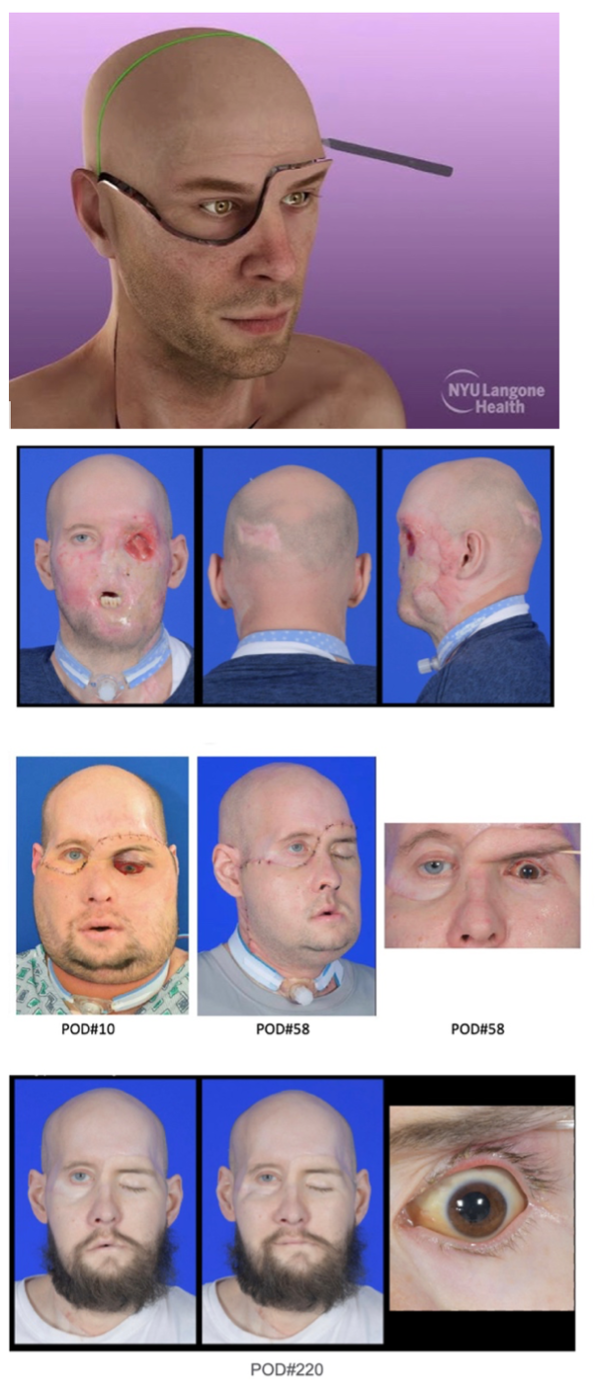
Introduction: The first successful human whole eye transplant (WET) performed concomitantly with a partial face transplant was performed in May 2023. The patient was a 46-year-old male who sustained a high voltage electrical injury resulting in severe mid and lower facial injuries and left eye enucleation. cPRA was 32%. Utilization of personalized surgical cutting guides and a novel anastomotic vascular bypass to ensure adequate perfusion of the globe during a combined FT/WET operation were key to the technical success.
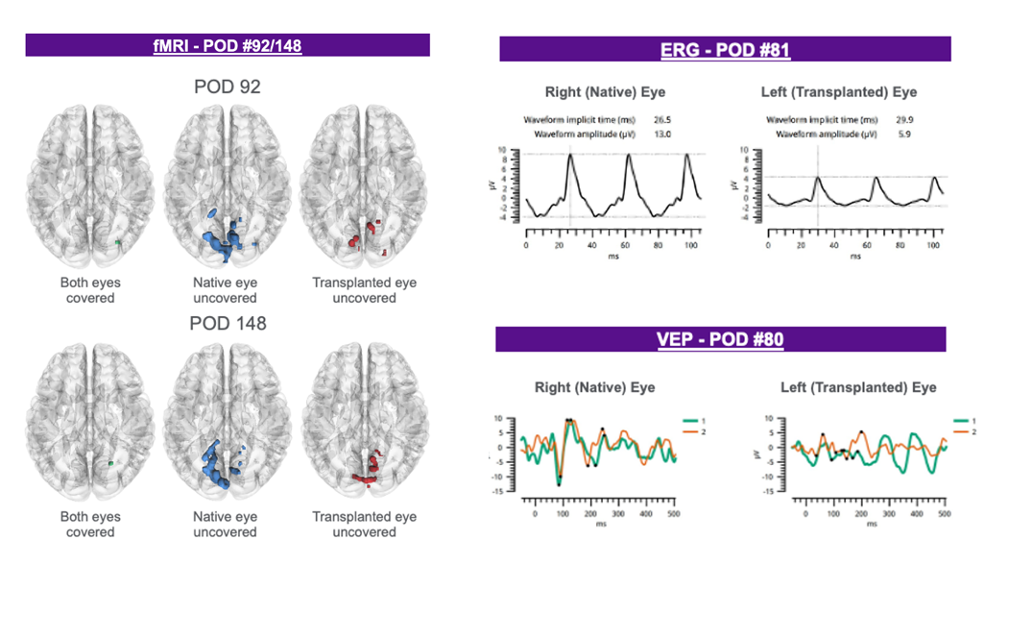
Methods: The combined partial face and whole eye transplant with optic nerve coaptation was performed in a 22-hour operation. Total ischemia time was 2hr59min. Induction immunosuppression included corticosteroids, rituximab, and thymoglobulin. Maintenance immunosuppression is standard triple therapy with tacrolimus, mycophenolate and prednisone. A novel vascular bypass using the superficial temporal artery and vein (STA/STV) maintained vascular flow to the globe via the external carotid vessels in order to minimize globe ischemia following transection of the ophthalmic artery. Donor derived CD34+ stem cells were injected, locally, at the site of optic nerve coaptation for their potential role in immunomodulation and nerve regeneration. Electroretinography (ERG), visual evoked potentials (VEP), and fMRI were utilized to evaluate the transplanted eye, retinal function, and optic nerve activity. Periodic surveys assessing psychological and social health were administered.
Results: Waitlist time was 107 days. Hospital discharge occurred at day 25. At 1 year, there have been no acute rejection, infectious episodes, de novo DSA production, or other adverse events. Evaluation and imaging of the face and eye demonstrates robust vascular perfusion to the face and globe, including the choroid and retina via the external carotid artery. Clinical assessment demonstrates a normal appearing transplanted eye with normal intraocular pressure. Anatomic imaging demonstrates retinal cell layer integrity and persistent laminar arrangement with a visible photoreceptor layer. Functional evaluation of the transplanted eye demonstrates evidence of function of the transplanted retina in response to light stimulus. fMRI demonstrates corresponding cortical activity at the visual cortex. To date, sight has not been restored. Psychological surveys have shown an increase in self-esteem and self-perception of image.
Conclusions: This successful transplant sets new benchmarks for reconstructive VCA options for severe disfigurement through progressive innovation offers tangible hope to those with previously irreparable facial and ocular deficits.
The world’s first combined partial face and whole eye transplant including optic nerve coaptation and local CD34+ stem cell application is free of acute rejection or adverse events to date. Aesthetic outcome and functional recovery continue to improve. Self-esteem and self-perception have improved with transplant.
[1] Eye Transplantation
[2] VCA

right-click to download
