
Long-term clinical outcomes in deceased donor kidney transplantation: A single-center experience
Woo Yeong Park1, Jaeseok Yang1, Jin Kyung Kwon1, Yaerim Kim1, Jin Hyuk Paek1, Kyubok Jin1, Seungyeup Han1.
1Division of Nephrology, Department of Internal Medicine, Keimyung University School of Medicine, Keimyung University Dongsan Hospital, Daegu, Korea
Introduction: Deceased donor kidney transplantation (DDKT) remains important despite the fact that its long-term survival rate is lower than that of living donor KT. Therefore, it is necessary to understand the factors related to allograft survival in DDKT. We aimed to evaluate long-term clinical outcomes and factors related to allograft survival in DDKT.
Method: This study included 500 patients who received KT from deceased donors at Keimyung University Dongsan Medical Center between October 1997 and October 2017. We investigated graft and patient survival rates, causes of graft failure and patient death, risk factors associated with graft failure, clinical characteristics according to HLA mismatch number, immunosuppressive agents, and graft failure.
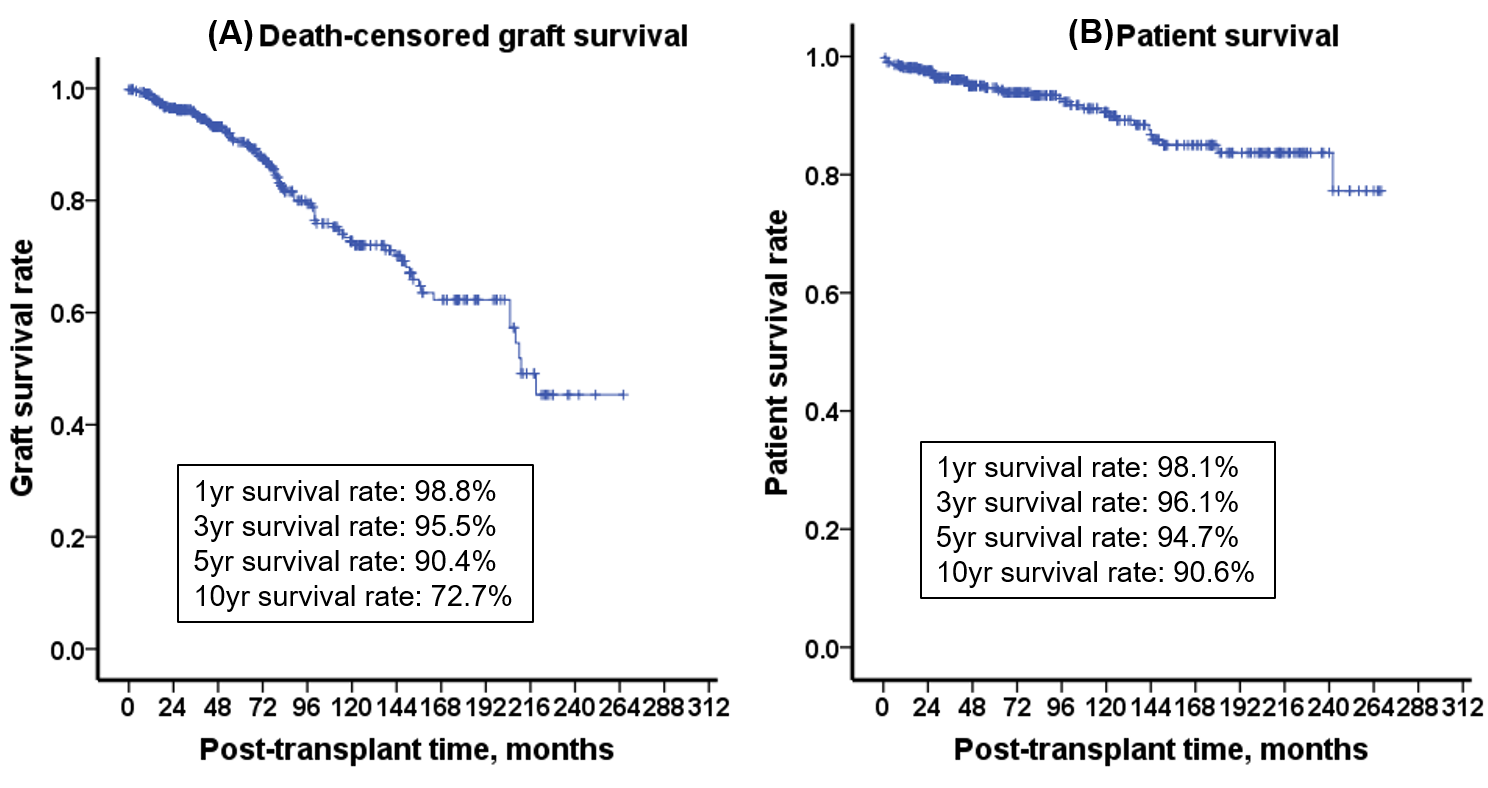
Results: Follow-up duration was 93.1 ± 70.8 months. Death-censored graft survival rates of 1-year, 3-years, 5-years, 10-years, and 20-years were 98.8%, 95.5%, 90.4%, and 72.7%, and 45.3%, respectively. The causes of graft failure were rejection (67%), patient death with a functioning graft (18%), recurrent glomerulonephritis (5.2%), and infection (5.2%). Patient survival rates of 1-year, 3-years, 5-years, 10-years, and 20-years were 98.1%, 96.1%, 94.7%, 90.6%, and 83.7% respectively. The causes of patient death were infection (61%), cardiovascular disease (11%), cerebrovascular accident (5.6%), and malignancy (2.8%). On multivariate analysis, serum creatinine levels at 1 year after KT, incidences of acute and chronic rejection, viral infections, and HLA mismatch number were independent risk factors related to allograft failure in DDKT. As the HLA mismatch number increased, the death-censored graft survival rate became significantly lower; however, there were no significant differences with respect to types of induction and maintenance immunosuppressant. Allograft function at 1 year after KT in the graft failure group was significantly lower than that of the non-graft failure group. The incidences of acute and chronic rejection, viral and bacterial infections were significantly higher in the graft failure group than in the non-graft failure group.
Conclusion: The independent factors associated with low allograft survival rate were low allograft function at 1 year after KT, high rejection rate, HLA mismatch number, and viral infection. To improve the allograft survival rate in DDKT, careful monitoring for allograft function during the early period after KT and HLA mismatch number, and maintenance of stable balance of immunologic status between rejection and infection are required.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Science and ICT, MSIT) (2021R1F1A1061572).
[1] Kidney transplantation
[2] Graft dysfunction
[3] Graft rejection
[4] Graft survival
[5] Patient survival
