The association of phase angle with in-hospital complication after laparoscopic living-donor hepatectomy
Gaabsoo Kim1, Yu Jeong Bang1.
1Anesthesiology and pain medicine, Samsung medical center, Seoul, Korea
Introduction: Donor safety and successful recovery are paramount in living donor liver transplantation (LDLT), given the potential risks to healthy donors. Various screening tools, such as frailty indices and nutritional markers, have been developed to identify patients at increased risk for postoperative adverse events. Phase angle (PA) measurements obtained through bioelectrical impedance analysis (BIA) reflect hydration status, muscle mass, and strength, and have been recognized as a promising marker of health status, frailty, and nutritional status, with potential predictive value for postoperative outcomes in different surgical contexts. This study hypothesized that lower preoperative PA would predict in-hospital adverse postoperative outcomes.
Method: This prospective randomized study was conducted at Samsung Medical Center in Korea between May 2023 and October 2023. Forty-four adult donors with an American Society of Anesthesiologists (ASA) Physical Status classification I–II who underwent elective laparoscopic hepatectomy were enrolled. Each patient underwent BIA, including PA assessment before surgery (PApre) and one day after surgery (PApost). Demographic and baseline data were extracted from electronic medical records. The day before surgery, experienced investigators performed BIA measurements and ultrasound examinations for diaphragmatic thickness fraction. The primary outcome was the association of PA with a composite of in-hospital complications after donor hepatectomy, including surgical complications, postoperative pulmonary complications, ileus, and acute kidney injury.
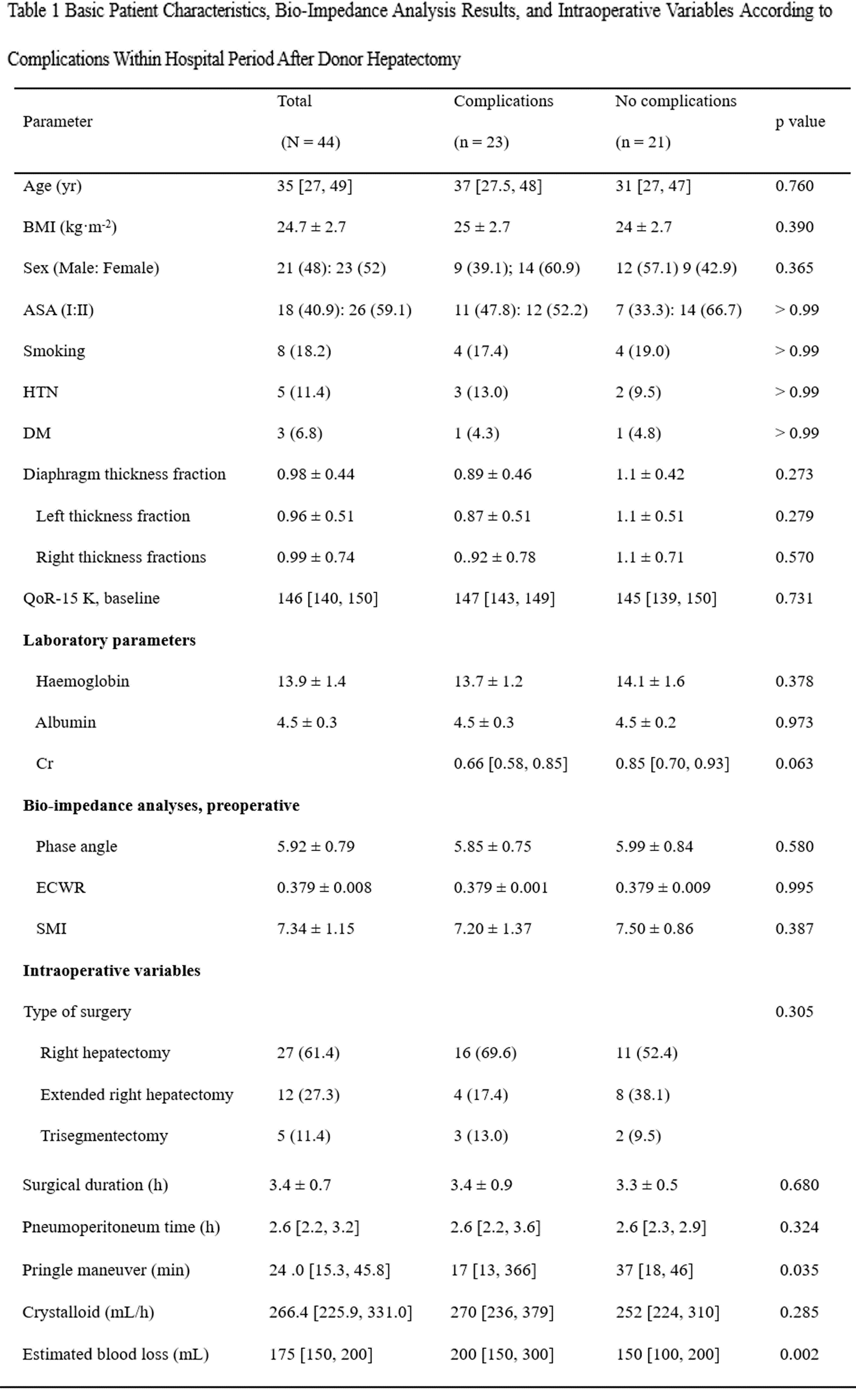
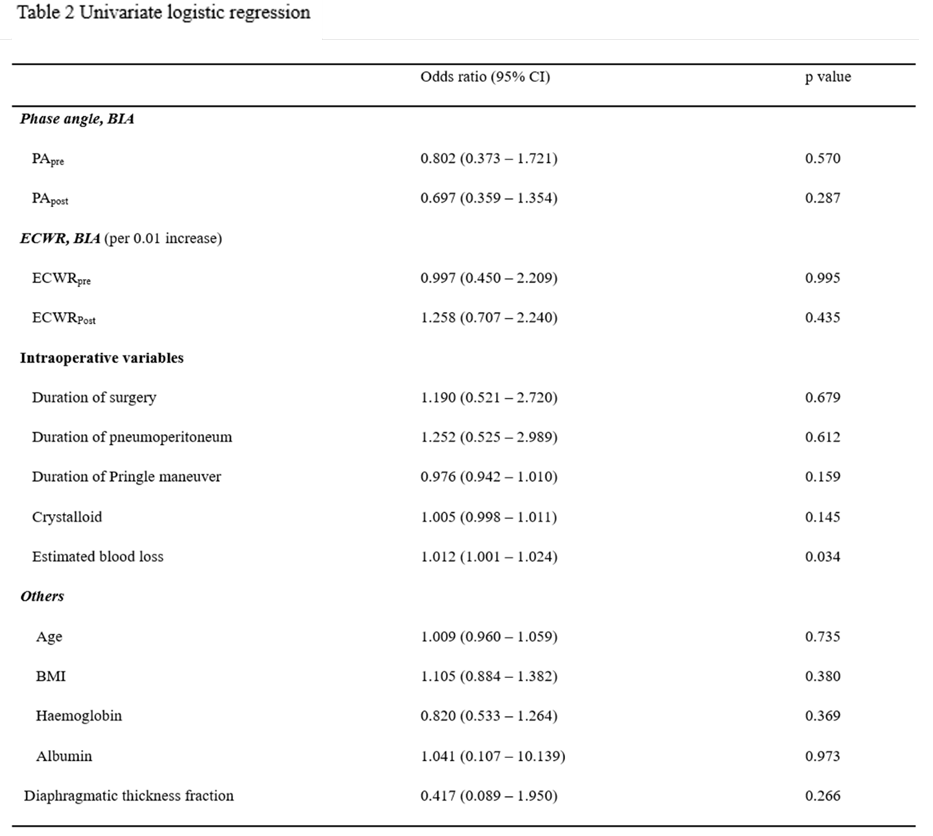
Results: The median age of participants was 35 years [27, 49], with 21 (48%) patients being male. Nearly half of the patients experienced one or more postoperative complications during their hospital stay. Baseline characteristics and preoperative BIA data according to variables included in in-hospital complications are presented in Table 1. There were no significant differences in baseline characteristics and PA between patients with or without complications, except for estimated blood loss during surgery. Logistic regression analysis (Table 2) was performed to assess the association of perioperative variables with postoperative complications, including age, BMI, laboratory results (hemoglobin, albumin, and creatinine), intraoperative variables (duration of surgery, pneumoperitoneum, pringle maneuver, crystalloid infusion, and estimated blood loss), and BIA (PA and extracellular water ratio). However, no significant risk factors were identified to predict postoperative complications.
Conclusion: Preoperative PA obtained from BIA measurements did not predict in-hospital complications after donor hepatectomy.
[1] Living-donor hepatectomy
[2] Postoperative complication
[3] Bio-impedence analysis
[4] Phase angle
