Comparison of renal volumetry and histological features between standard and marginal donors
Shunta Hori1, Mitsuru Tomizawa1, Kuniaki Inoue1, Tatsuo Yoneda1, Kenta Onishi1, Yosuke Morizawa1, Daisuke Gotoh1, Yasushi Nakai1, Makito Miyake1, Kiyohide Fujimoto1.
1Urology, Nara Medical University, Nara, Japan
Introduction: Detailed criteria of living kidney donors (LKDs) have been still controversial in Japan, where living donor kidney transplantations are common because of the severe shortage of deceased donor sources. Transplant centers and surgeons are responsible for making decision considering balance the potential LKDs desire to donate against their future risk of end-stage renal disease and associated morbidity. In this study, the roles of volumetry and scintigraphy for preoperative and postoperative renal function were investigated and the association of volumetry and scintigraphy with the early recovery of residual renal function (RRF) was evaluated.
Method: We included 128 LKDs who underwent donor nephrectomy (DN) at our institution between 2006 and 2022 and whose tissues were available. Clinical and radiographic data were retrospectively obtained from their medical charts. Renal volume parameters were calculated using the preoperative computed tomographic images in the Volume Analyzer SYNAPSE VINCENT image analysis system. Tissues obtained from allograft biopsy were examined. Marginal donors were defined according to Japanese guideline.
Results: LKDs were divided into two groups; 89 as standard donors (SDs) and 39 as marginal donors (MDs). The median age and estimated glomerular filtration rate (eGFR) were 56 years and 80.7 mL/min/1.73m2 in SDs and 64 years and 72.2 mL/min/1.73m273 in MDs, respectively (P=0.0012 and P=0.031). Parameters calculated by renal volumetry were not significantly different between the two groups, while interstitial inflammation and interstitial fibrosis/tubular atrophy were significantly higher rate in MDs than those in SDs (P=0.031 and P=0.041). Multivariate analysis revealed that age <60, body mass index >25, residual kidney volume/body surface area (RKV/BSA) were independent factors for poor renal function preservation (odds ratio [OR] 2.56, 95% confidence interval [CI] 1.06–6.16; OR 2.99, 95%CI 1.11–8.05; OR 4.11, 95%CI 1.70–9.96, respectively). Subgroup analysis involved in MDs revealed that RKV/BSA and arteriosclerosis were independent factors for poor renal function preservation (P=0.010 and P=0.025). Furthermore, with regard to graft survival in recipients, recipients donated from MDs were significantly high risk of graft loss compared with those from SDs (P=0.0019).
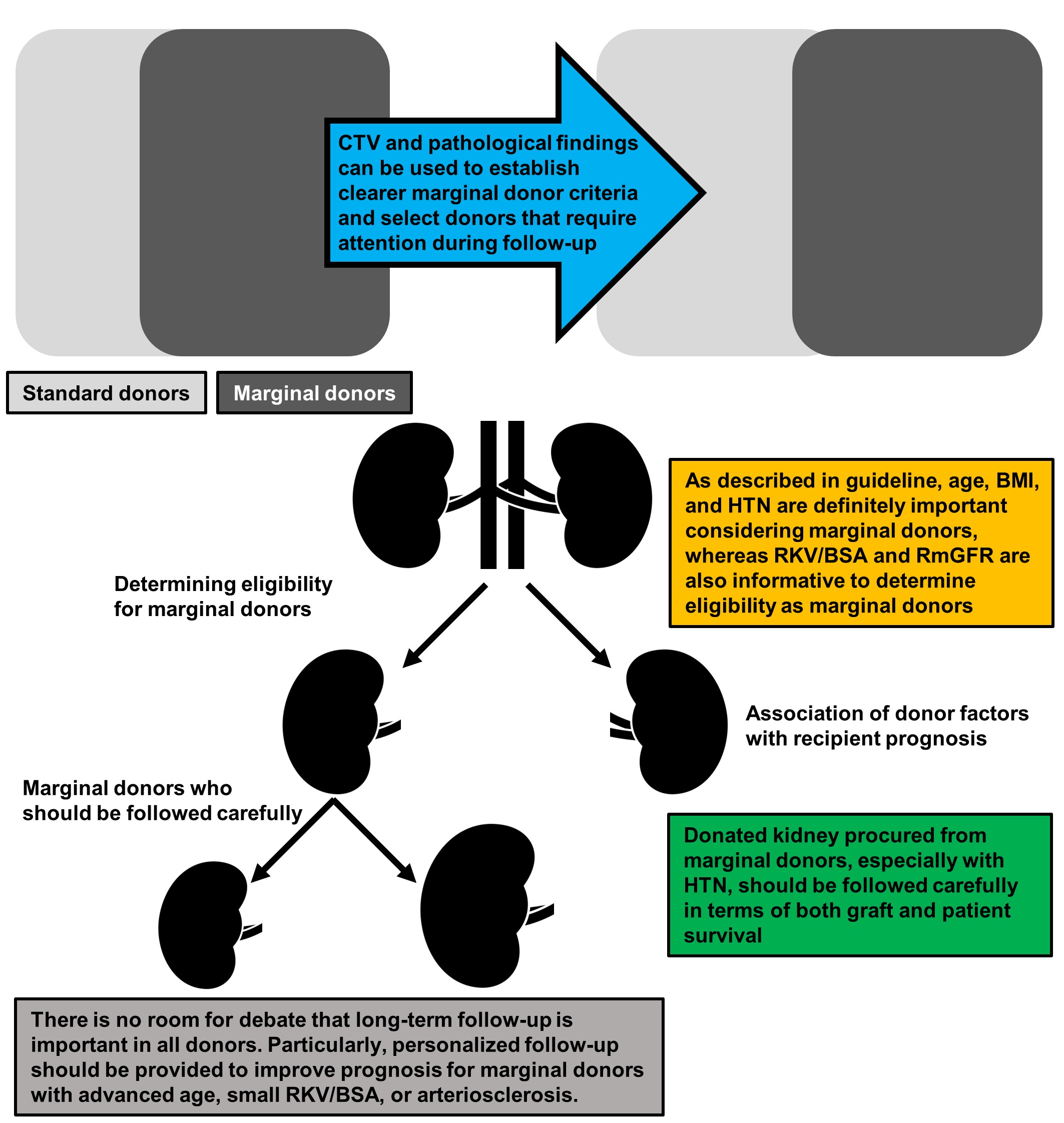
Conclusion: Our findings suggest that RKV/BSA calculated by volumetry can be a reliable screening and prognostic tool for choice of LKDs including MDs, and RKV/BSA and histological findings such as arteriosclerosis can be used to establish clearer MD criteria, leading to optimal and personalized follow-up after DN (Figure 1). Further investigation is needed to establish systematic criteria for LKDs in Japan.
[1] living donor kidney transplantation
[2] marginal donor
[3] residual renal function
[4] graft survival
[5] volumetry
[6] arteriosclerosis
