Clinical characteristics of lupus nephritis patients submitted to kidney transplantation in a single center
Beatriz Pachi2, Laura Bischoff2, Luísa Borba2, Helena Bischoff2, Gisele Meinerz1,2, Elizete Keitel1,2.
1Nephrology and Kidney Transplantation, Santa Casa de Porto Alegre, Porto Alegre, Brazil; 2Departamento de Clinica Medica, UFCSPA, Porto Alegre, Brazil
Background and Objectives: Lupus Nephritis (LN) affects approximately 50% of patients with Systemic Lupus Erythematosus (SLE), and can lead to end-stage renal disease requiring kidney transplantation. This study aimed to evaluate patient demographic data, post-transplant clinical evolution, complications and renal survival.
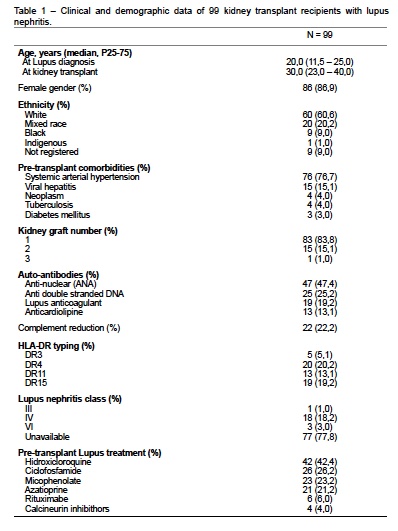
Methodology: Retrospective cohort of 99 kidney transplant recipients due to LN from 1977 to 2023 in a single center.
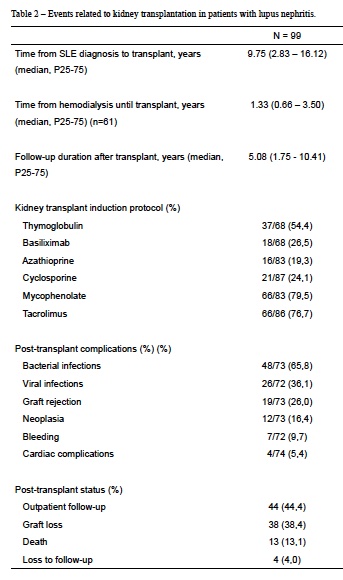
Results: The patients were mostly white (65.9%), female (86.9%), submitted to their first kidney transplant (83.8%). Median age at SLE diagnosis was 20.0 (11.5 – 25.0) years and 30.0 (23.0 – 40.0) years at transplantation. 84.4% were hypertensive. The histological classification of LN was recorded in 22% of the patients, mostly class IV (18.2%). LN treatment included hydroxychloroquine (47.7%), cyclophosphamide (29.2%), mycophenolate (25.8%) and azathioprine (23.6%). Regarding the extrarenal manifestations of SLE, there was a significant reduction in joint symptoms [71% vs 52.9%, OR 0.70 (0.010 - 0.472), p < 0.001], mucocutaneous symptoms [70.6% vs 52.9%, OR 0.026 (0.004 - 0.183), p < 0.001] and neurological [12.1% vs 8.1%, OR 0.046 (0.014 - 0.153), p < 0.001] before and after RT, respectively. There was no difference in the occurence of thrombotic, obstetric, ophthalmological and serositis events. The presence of lupus anticoagulant and anticardiolipin antibody alone or in combination was not associated with pre-KT thrombosis, nor post-KT thrombosis or bleeding. Table 2 shows the most frequent complications after KT. Graft loss occurred in 38.4% of patients, and death with a functioning graft in 13% (4 patients died of COVID-19). The 5-year graft survival was 71.6% and there was no recurrence of LN. The presence of HLA DR15 was associated with a shorter time between SLE diagnosis and initiation of dialysis [41.0 (12.0 - 155.0) vs 117.5 (17.2 - 198.7) months, p = 0.042] and with a higher risk of graft loss (HR 3.34 CI 95% 1.06 - 10.57, p = 0.040). Male sex was also associated with a higher risk of graft loss (HR 4.21 CI 95% 1.08 - 16.38, p = 0.038).
Conclusion: We presented the clinical charactistics and outcomes of 99 patients with LN submitted to KT. The extrarenal manifestations of SLE tend to reduce post-transplant. Post-transplant graft survival was similar to that of kidney transplants for other causes at this institution. The presence of HLA DR 15 and male sex appear to be associated with greater graft loss in LN patients.
[1] kidney transplantation
[2] lupus nephritis
[3] systemic lupus erythematosus
