Mycotic aneurysms in intestinal transplantation: A case series
Nicola Colucci1, Harry VM Spiers1, Georgios Geropoulos1, Neil K Russell1, Andrew Winterbottom2, Sara Upponi2, Andrew J Butler1, Irum Amin1.
1The Roy Calne Transplant Unit, Department of Surgery, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom; 2Department of Radiology, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom
Introduction: Mycotic aneurysms (MA) represent a potentially fatal complication following solid organ transplantation. The risk of developing MA is higher in the context of Intestinal Transplantation (ITx), likely arising from several factors such as utilization of aortic conduits, the nature of the explant (e.g., chronic abdominal sepsis), potential for contamination of the vascular graft during enteric anastomoses and the heightened burden of immunosuppression.
Methods: This is a retrospective review of a prospectively held database of all adult ITx from December 2007 to March 2024.
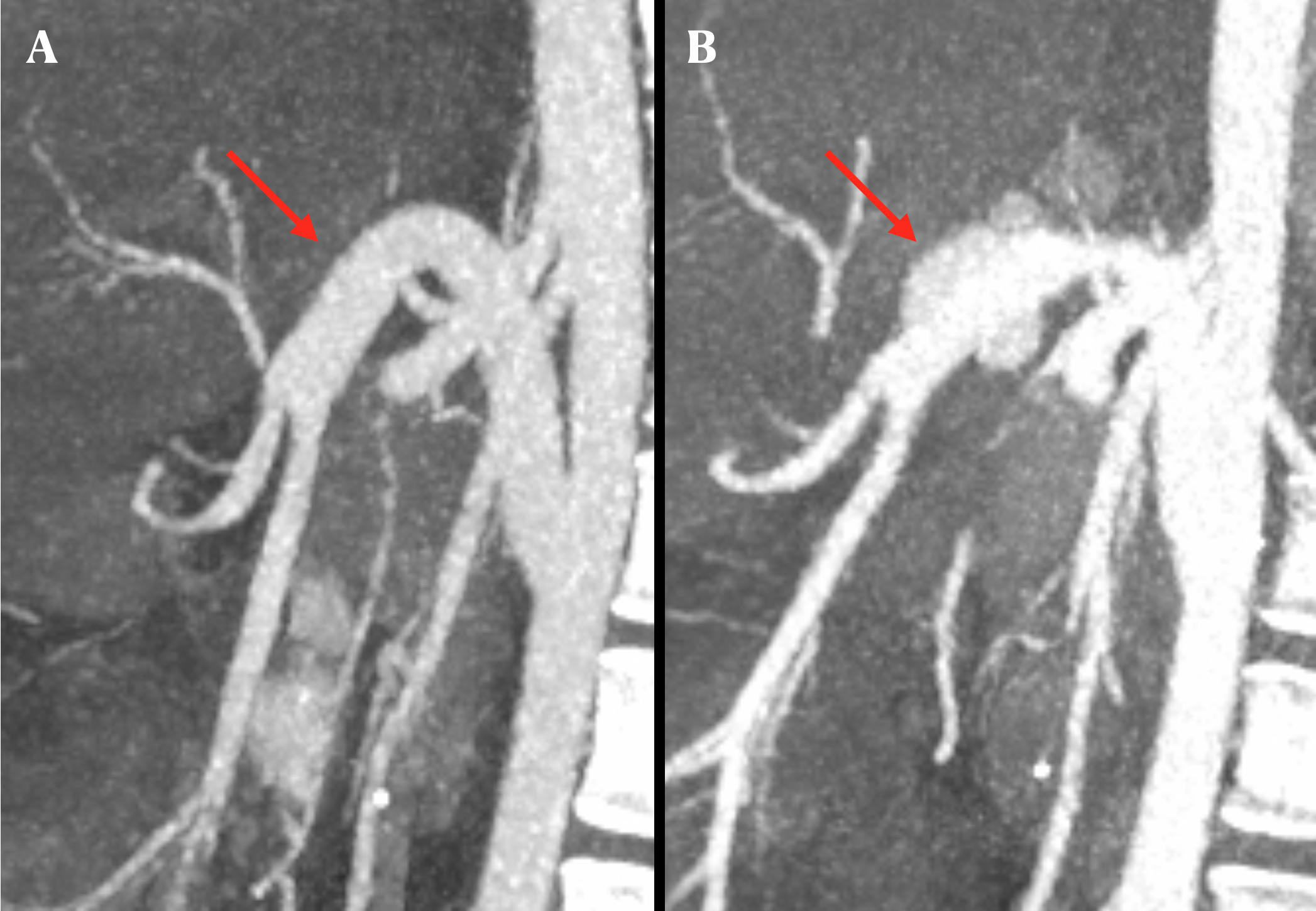
Results: Out of 156 ITx performed, six patients (3.8%) experienced eight episodes of MA. Among them, four patients received a multi-visceral transplant, while two underwent a liver-small bowel transplant, all vascularised with infra-renal aortic conduits. The median age at MA diagnosis was 36.5 years (range 24-70), occurring bimodally either early post-transplant (2, 3, 6, 8 weeks) or in a later phase (55, 377 weeks). Two patient experienced recurrence, occurring on average 132.4 weeks from the initial diagnosis (range 69.6-195.3). A history of hollow viscus perforation or anastomotic leak after transplant was identified in all cases except one (83.4%). Diagnosis was made peri-operatively in two cases (33.3%) due to ruptured aneurysms necessitating urgent laparotomy, while the remaining cases were diagnosed via angio-CT (Figure 1), typically in the context of abdominal pain and ongoing sepsis.
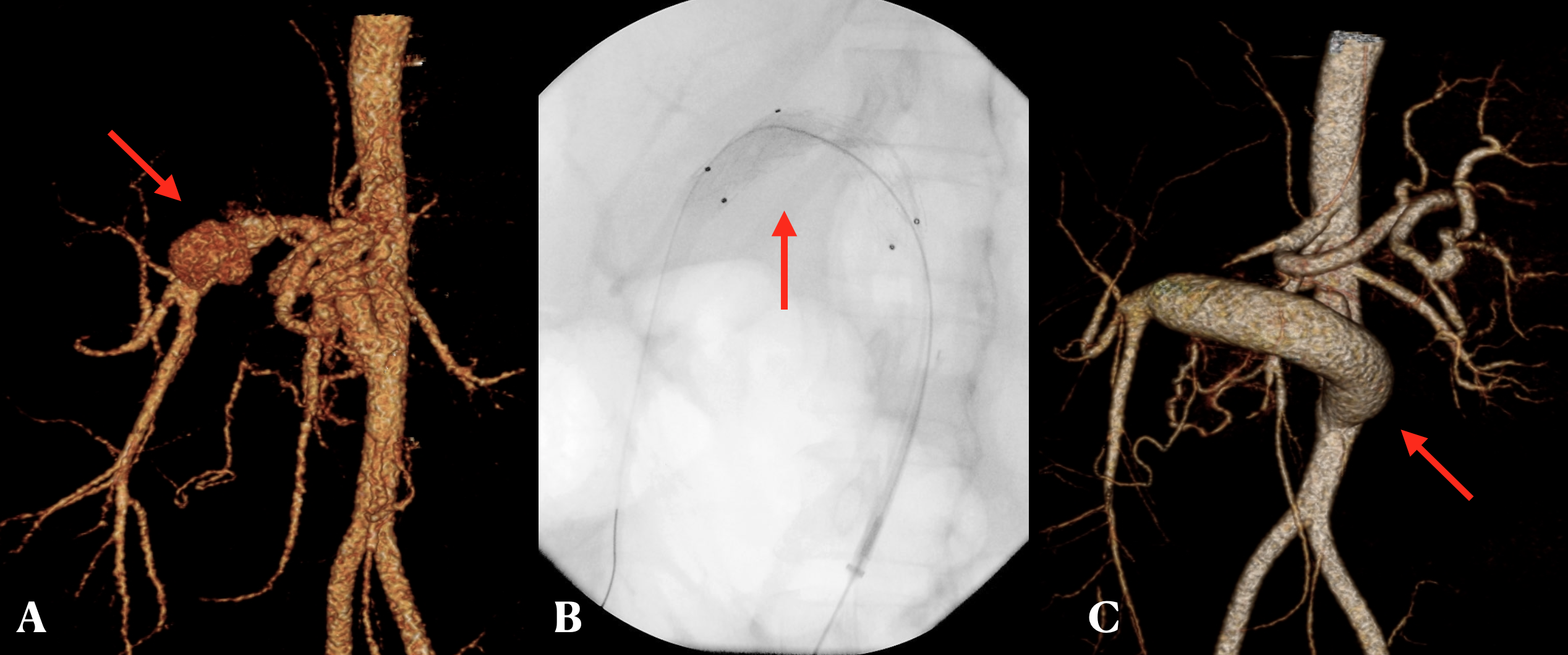
The two recurrences were clinically more subtle, identified incidentally on a CT in one case or associated with abdominal discomfort and maelena in the other. Apart from targeted antibiotic and antifungal treatment, management strategy pivoted around endovascular stent grafting (ESG) followed by a subtotal resection of the aneurysmal vessel and creation of a new conduit (Figure 2) using third party vascular homograft.
Mortality occurred in 83.4% of patients, with 50% of deaths within the first week after diagnosis. Two patients survived both the initial episode and also a recurrence, with one remaining alive and well five years after the first diagnosis.
Conclusion: MA of the aortic conduit in the setting of ITx is a relatively uncommon complication associated with high mortality. Its occurrence is often linked to a history of hollow viscus perforation or anastomotic leak. Diagnosis typically relies on angio-CT but may occur peri-operatively during catastrophic bleeding from aneurysm rupture. Treatment should entail ESG followed by conduit resection. Early aggressive control of potential contamination sources after ITx is paramount, although drawing general conclusions is limited by the low absolute incidence of this condition.
