Fast track living donor protocol for pediatric liver transplant, the speed that saved lives
Valeria Ramirez Rios1, N. Monserrat Arreola G 2, J. Manuel Zertuche C2, Yuridia L. Plascencia G2, Elizabeth Hernández-Chávez3, Sergio Pacheco3, Norma L Valdez A4.
1Pediatric Surgery Department, Pediatric Hospital CMNO IMSS, Guadalajara, , Mexico; 2Uro-Nephro-Transplant, Pediatric Hospital CMNO IMSS, Guadalajara, , Mexico; 3Gastroenterology, Pediatric Hospital CMNO IMSS, Guadalajara, , Mexico; 4Social Services Department, Pediatric Hospital CMNO IMSS, Guadalajara, , Mexico
Introduction: Acute liver failure (ALF) is defined as the incapacity of the liver to fulfill it´s biosynthesis, regulation, and detoxification functions, > to 50% of the cases of ALF can be of undetermined etiology (UE), having a lower rate of spontaneous recovery, higher chances of requiring transplant, and higher mortality than other etiologies. It´s priority relies in the early assessment of indication of liver transplant (LT), the only treatment with a clear benefit on mortality in severe ALF.
Method: Case series study of fast-track living donor transplant protocol (F-TLDTP) that occurred in January 2024 in a high-specialty pediatric hospital in Guadalajara, Mexico.
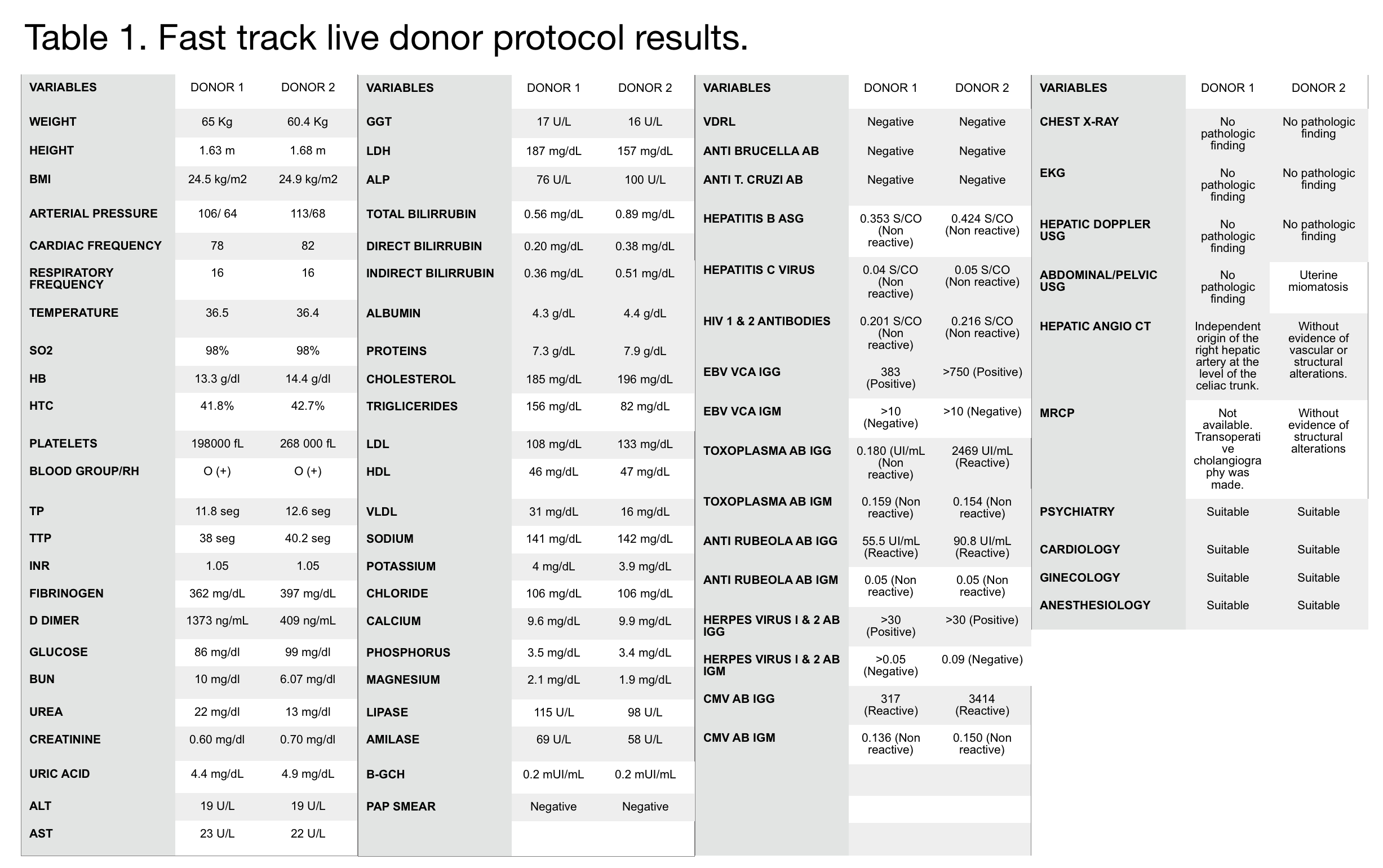
Results: 2 females between 3 and 4 years of age, arrived at the emergency department with ALF, initiating medical management, in their studies with inconclusive results, so ALF was classified as of UE. A few hours after arriving at the hospital, they showed clinical worsening and were admitted to the pediatric intensive care unit. Reaching grade IV encephalopathy and requiring advanced airway management, hemodynamic instability requiring the use of vasoactive amines and use of slow renal replacement therapy (PRISMA). They were placed on the zero-liver urgency (ZLU) for a waiting list, without a positive response in the first 24 hours. Time was against us and in order not to waste any more time it was decided to start the F-TLDTP, consists of determining compatibility, metabolic, infectious, and imaging studies, evaluations by different specialties to determine that the donor is healthy, suitable and agrees to donate an organ. The protocol began with the parents. In case 1, the mother was ruled out due to obesity and the father due to ABO incompatibility, the maternal aunt was studied, compatible and agreed to be a living donor (LD). In the second case, we initially study the mother, being compatible and accepting the donation. The F-TLDTP are shown in Table 1. An extraordinary job was done, completing this protocol, Liver Transplant Living Donor (LTLD) was performed successfully in 3 days.
Conclusion: Given the shortage of pediatric organ donation, LD donation to ZLU should be considered. If we wait for an organ with the same characteristics between donor and recipient, LT would not be possible. Its our obligation to present to parents the possibility of donating and thus optimize times, control risk factors, reduce cold ischemia, which together improves the survival of patients at ZLU. Even in these cases, in which ALF of undetermined etiology occurred, LT is the only option to save the patient's life. This work is of clinical importance as it shows how by acting quickly, with the support of the entire multidisciplinary team involved in patient care, LTLD can be performed. We present the first report of an F-TLDTP for pediatric recipients in ALF, a fast, timely and safe way to obtain a liver.