
The impact of preformed donor specific antibodies (DSAs) on outcomes of simultaneous liver-kidney (SLK) transplant recipients
Hasan Khamash1, Caroline Jadlowiec2, Blanca Lizaola-Mayo1, Pooja Budhiraja1, Sami Alasfar1, Raymond Heilman1, Bassam Abu Jawdeh1, Hay Me Me1, Bashar Aqel1, Kunam Reddy2, Amit Mathur2.
1Medicine, Mayo Clinic Arizona, Phoenix, AZ, United States; 2Surgery, Mayo Clinic Arizona, Phoenix, AZ, United States
SLK transplant recipients have excellent outcomes that rival kidney alone recipients in terms of graft and patient survival and have better outcomes in terms of rejection rates both the cellular and the antibody variants. It is mandatory to obtain a crossmatch prior to SLK transplant but not uncommonly a transplant will proceed with only a virtual crossmatch.
Aim: Assess the effect of the presence of DSA or positive FCXM on outcomes.
Method: This is a retrospective single center study including all SLK recipients from January, 2017 to December, 2022. 122 patients were included in this study. 13 patients were excluded due to primary organ non function or death within 1 month. No cases with rejection were excluded. We do not exclude donor HLA antigens regardless of recipient sensitization. HLA antibody data was reviewed at time of transplant and on follow-up. Variables including graft and patient survival and function were tracked through November, 2023.
Results: 25 patients had DSA and out of those 15 had positive FCXM. 16/25 had cPRA>20% in the DSA group compared to 12/97 in the no-DSA group. 9 patients had Class I DSA, 11 Class II DSA, and 5 had both. Mean fluorescence intensity values ranged from 1000 - >20000. DSAs have resolved on post-transplant follow up in 12/23 patients and persisted in 11/23, 9 were class II DSAs. Rejection was more common in the DSA group although only 3/6 cases were due to preformed antibosies the remainder were due to cellular rejection in the setting of maintenance immunosuppression reduction. Antibody mediated rejection cases except for 1 were successfully treated. Immunosuppression induction was mostly with basiliximab except for 5 recipients with DSA received rATG. Maintenance was with tacrolimus, MMF, and prednisone which was tapered off unless DSAs were present.
| No-DSA (n=97) | DSA (n=25) | p value | |
|---|---|---|---|
| Age (yrs) | 59±11.2 | 59.6±9.8 | NS |
| Gender (F) | 31 (32%) | 9 (36%) | NS |
| Donation after cardiac death | 47 (48.5%) | 11 (44%) | NS |
| KDPI median | 38% (19%-51%) | 39% (22%-61%) | NS |
| Delayed graft function kidney | 37 (38%) | 7 (28%) | NS |
| Rejection kidney | 4 (4.3%) | 6 (24%) | 0.002 |
| Rejection liver | 6 (6.5%) | 4 (16.7%) | NS |
| Creatinine at follow-up | 1.26 ± 0.34 | 1.25 ± 0.3.2 | NS |
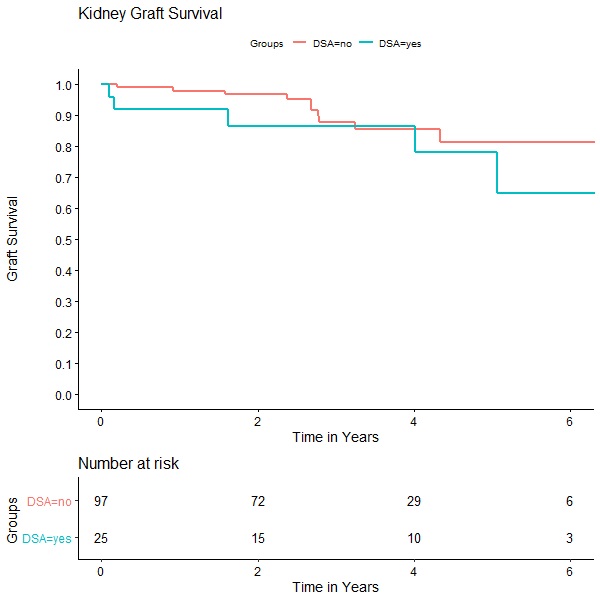
Conclusion: There was higher risk for rejection in the DSA group that did not impact patient and graft survival. At our center we do not list unacceptable antigens for SLK candidates.
[1] Simultaneous liver kidney transplant
[2] Allosensitization
[3] antibody mediated rejection
