Non-autogenous graft reconstruction in an external iliac artery dissection in a post-transplant recipient
Joseph Laygo1, James Angelo Illescas1, Adolfo Parayno1, Leo Carlo Baloloy1.
1Division of Organ Transplant and Vascular Surgery, National Kidney and Transplant Institute, Quezon City, Metro Manila, Philippines
Introduction: Vascular complications accounts to less than 10% of all complications in renal transplantation. A rare but potentially disastrous occurrence that can cause kidney and lower extremity perfusion loss is iliac artery dissection. Management of external iliac artery dissection (EIA) is poorly established and challenging.
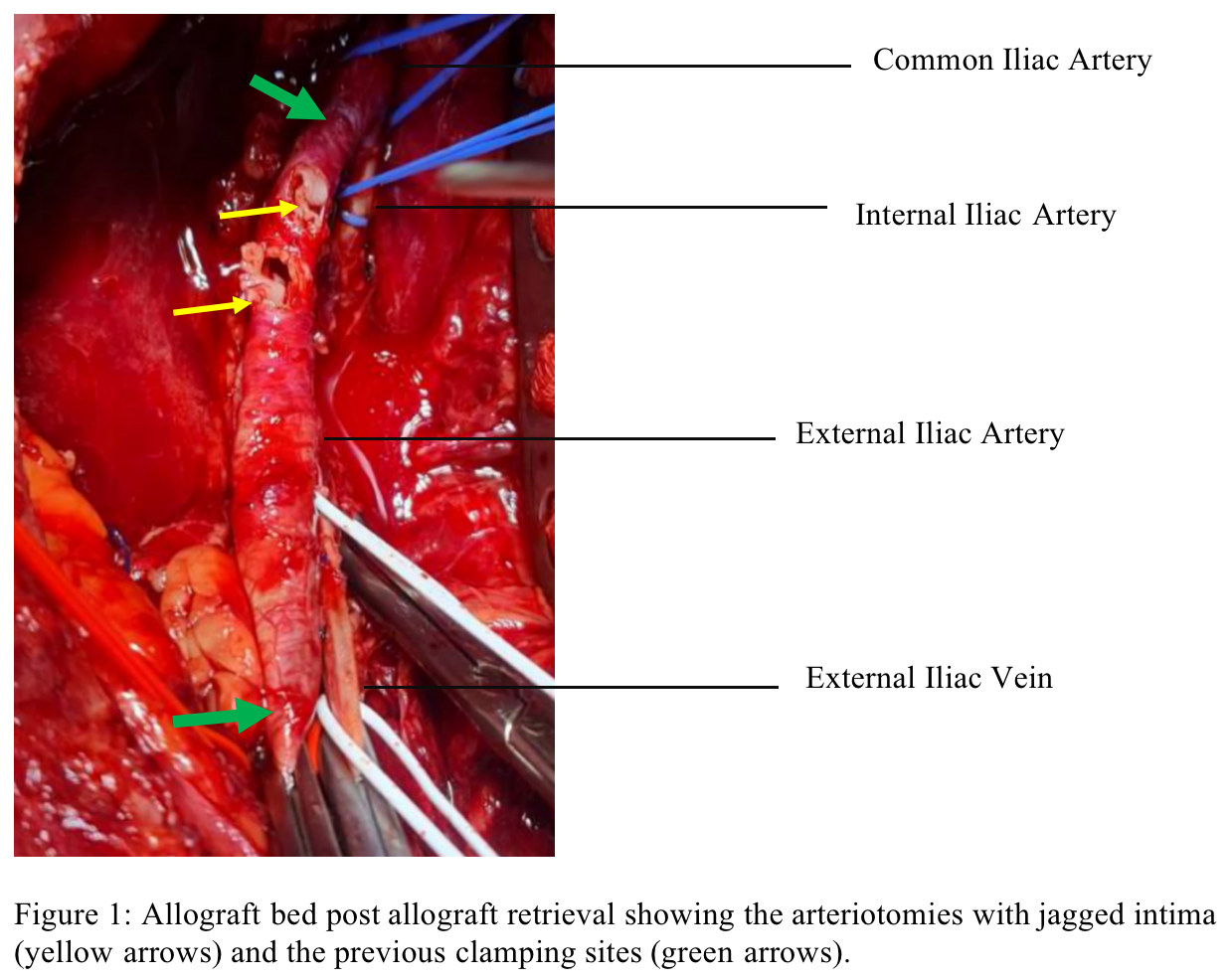
Case: This is patient C.A., a 53 year old male, diabetic and hypertensive, previous smoker, diagnosed with end-stage renal disease. Patient is on hemodialysis for five years who underwent renal transplantation. The allograft has two renal arteries, single vein and single ureter. The recipient’s external iliac artery(EIA) is tortuous, soft and smooth with no palpable plaques. The allograft arteries were anastomosed to the EIA thru an arteriotomy using 4.4mm puncher. Unclamping showed a well perfused renal allograft with thrill on both arterial anastomoses. Urine output was immediately observed. Patient's vital signs remained stable at the post-anesthesia care unit, after an hour, patient became oliguric. Despite adequate hydration and administration of diuretics, patient became anuric. At the 3rd post-operative hour, the recipient was re-operated. Intraoperatively, the allograft was soft and pale, thrill was palpated on the main renal artery, with questionable thrill on the accessory renal artery. Inspection revealed an ischemic posterior aspect of the allograft and violaceous clamp sites at proximal and distal external iliac artery. Clamping of the distal EIA was done to observe improvement of blood flow to the allograft, however, revealed persistent ischemia of the allograft and absence of thrill at the main renal allograft artery. Allograft was then explanted and re-perfused. Inspection of the EIA revealed separation of the intima at the clamp sites extending to the arteriotomies (Figure 1). EIA dissection was deemed irreparable hence, EIA was resected, and reconstruction using a 6mm Polytetrafluoroethylene (PTFE) graft was done (Figure 2).
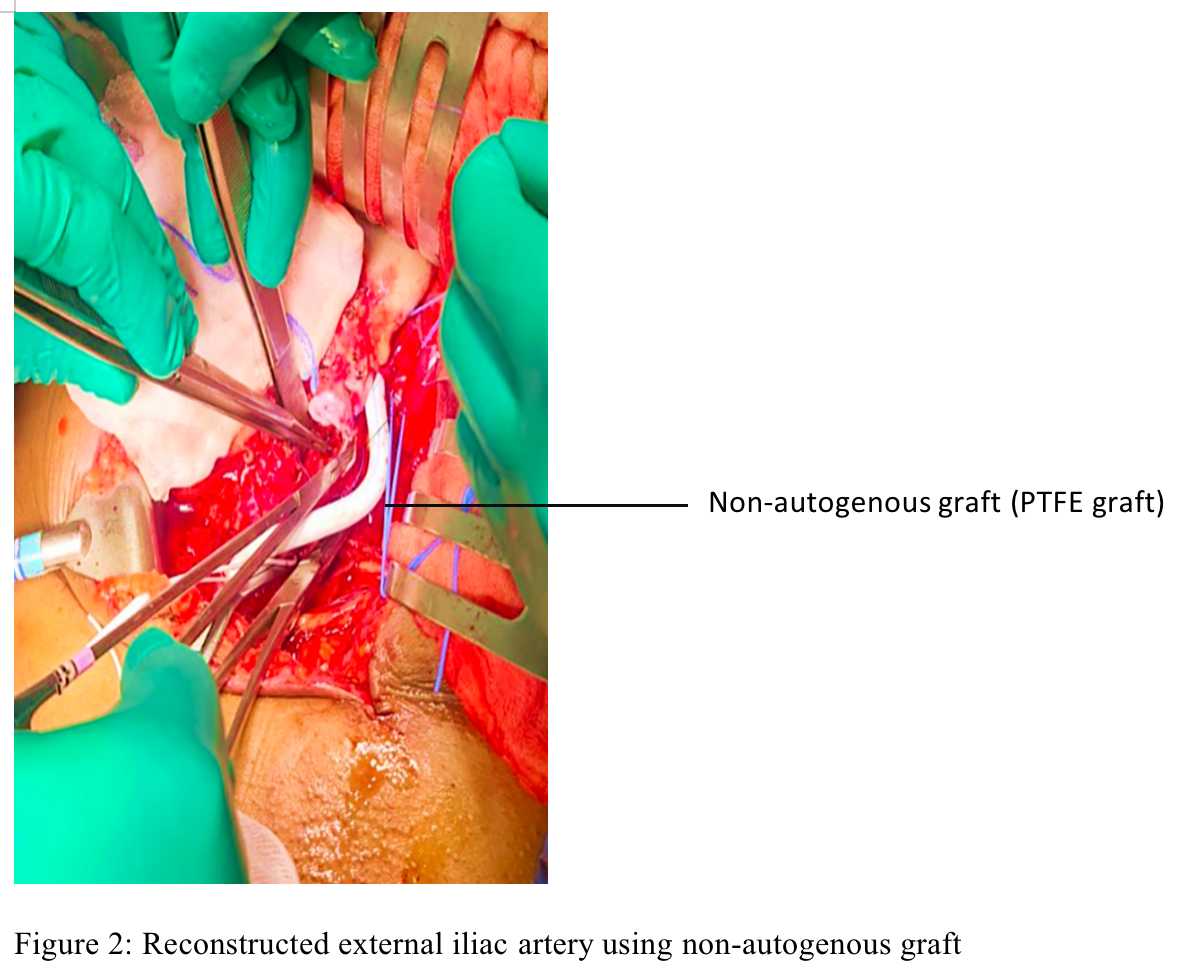
Arteriotomies were done using the 4.4 mm puncher thru the PTFE graft. Renal allograft arteries and vein anastomosed in an end to side technique. Following surgery, graft function improved with declining creatinine trend. The right lower extremity was unremarkable. Patient was discharged and maintained on anticoagulant after seven hospital days. Three months after transplant, the creatinine level is within normal range.
Conclusion: EIA dissection should be considered a differential diagnosis in cases of allograft dysfunction. It compromises the perfusion of the allograft and extremity. It entails a high degree of clinical suspicion, timely imaging and swift intervention. Using soft Fogarty clamps, clamping away from atherosclerotic calcifications, and meticulous suturing are some ways to prevent arterial dissection. In cases of irreparable arterial intimal injury, the use of non-autogenous graft is a crucial salvage technique.
