Challenges and opportunities: Early outcomes of elderly renal transplant recipients
Alex W Rogers1, Lillian W Gaber1, Edward A Graviss1, Ahmed O Gaber1.
1Houston Methodist Hospital, Houston, TX, United States
Introduction: Elderly patients are the fastest growing population of patients awaiting kidney transplant in the US, but have decreased post-transplant survival compared to younger recipients. Herein, we aim to evaluate early post-transplant outcomes of elderly kidney transplant recipients at a large volume center compared to younger recipients, and to describe the challenges in managing this cohort.
Method: Single-center, retrospective comparative cohort study in patients who received a kidney transplant between January and December 2022. Patients were excluded if they received a multi-organ transplant. Elderly was defined as age ≥70 years at the time of transplant. The primary endpoint was defined serum creatinine (SCr) at one-year post-transplant. Statistical analyses were conducted using χ2 and Fisher’s exact as appropriate.
Results: 190 patients were analyzed during the study period. Of these, 17 patients were ≥ 70 years old at the time of transplant. Baseline characteristics, aside from age, were similar between groups.
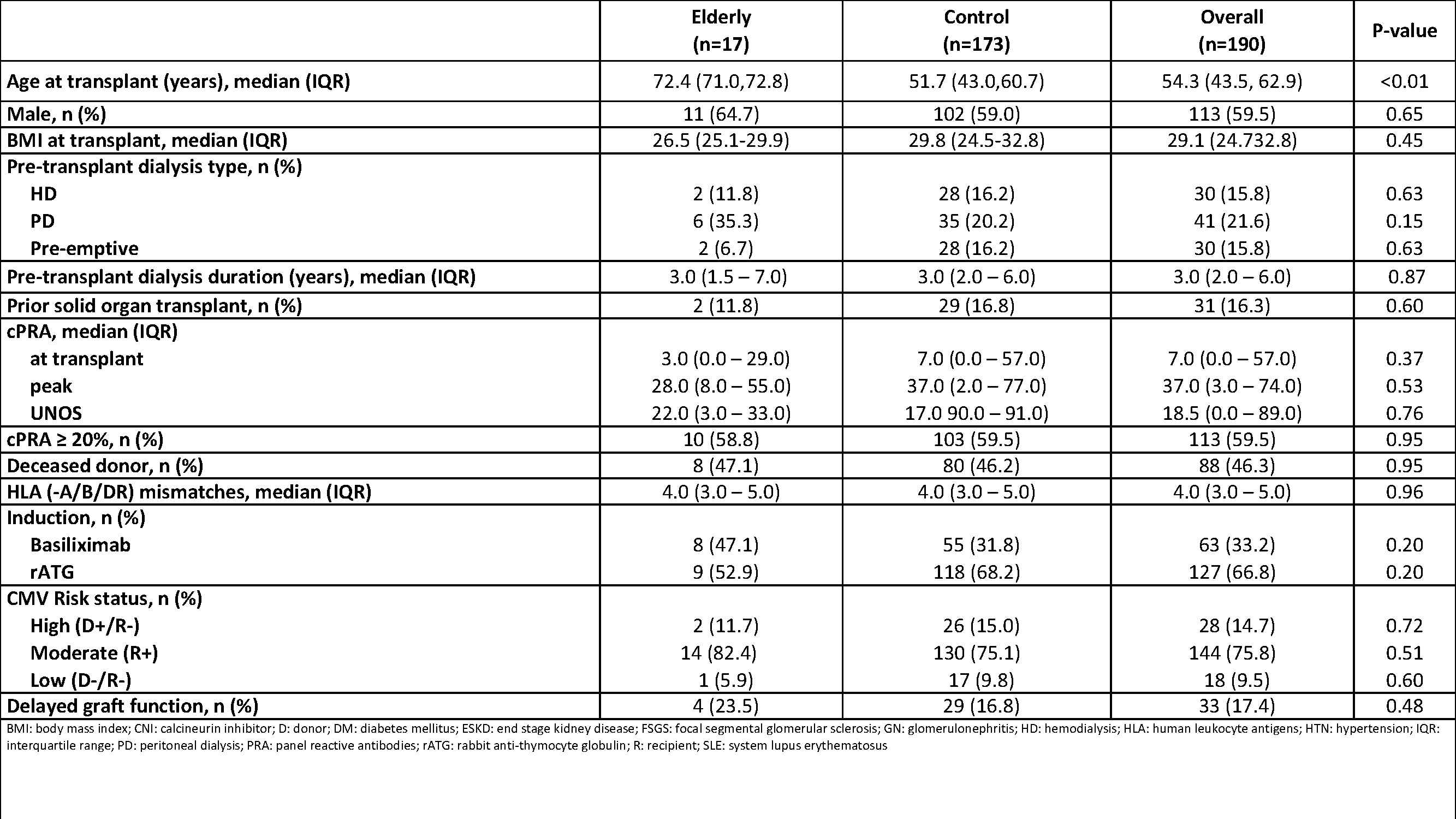
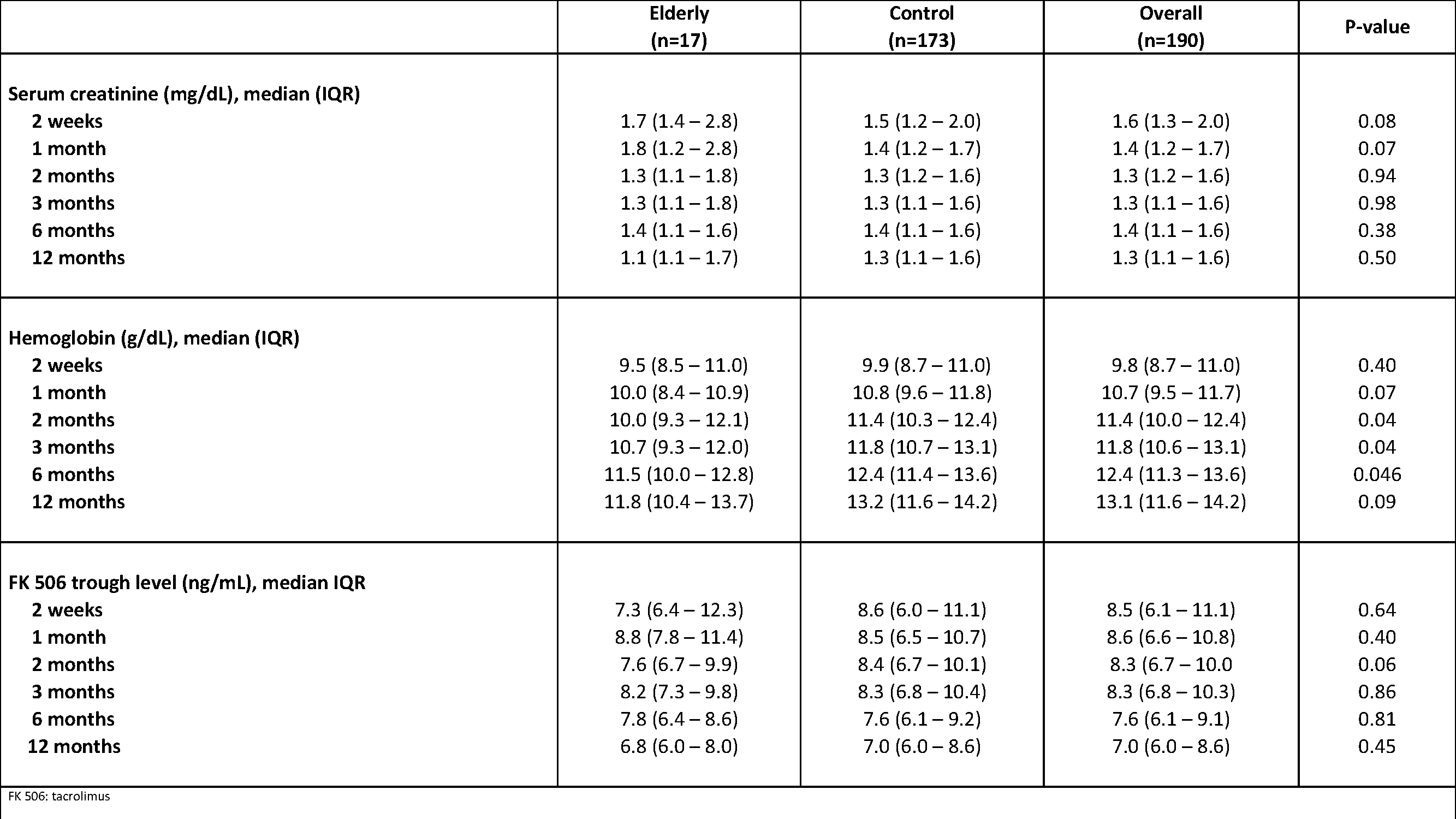
The majority of patients were male with ESKD due to diabetes or hypertension and on peritoneal dialysis prior to transplant for a median of 3 years. SCr at one year was equivalent between groups (1.1 vs 1.2; p=0.5), but elderly patients had a higher numerical SCr in the first month post-transplant. Elderly patients had a significantly lower hemoglobin months 2-6 post-transplant, but were similar at one year (11.8 vs 13.2, p=0.09). WBC and Platelets were similar between groups throughout the year and no significant differences in the incidence of BK, CMV, or patient and graft survival were observed. Rates of acute rejection at one year were 6.3% for elderly vs 12.5% in the control group (P=0.7); and de novo DSA development was 7.4% vs 13.3% (P=1.0).
Of the 17 elderly patients, one experienced early graft failure due to disease recurrence in the first month post-transplant. Of the remaining 16, 11 patients accounted for 12 ED visits and 31 hospitalizations in the first year following transplant. ED visits were most common for lab abnormality (33%) and drain/foley complications (25%). The predominant readmission indication was UTI (48%), respiratory tract infection (16%), and AKI (10%).
Conclusion: We observed similar one year renal function and graft outcomes overall, but with a significant utilization of higher level care during the first year for the elderly cohort, particularly for infection. Given the low rates of rejection in this group, further investigation into reduced immunosuppression exposure may be warranted.
