Analysis of the 7 years results of kidney transplantation program in the surgery center of Uzbekistan
Bakhritdinov Fazlitdin1, Matkarimov Zohidjon1, Akhmedov Akrom1, Suyumov Azamat1, Sobirov Jasur1, Zafarbek Abdugafurov1, Komilova Dildora1, Elmuradova Nigina1, Rustamov Muzaffar1, Urinov Jasur1.
1Kidney Transplantation, RSSPMCS named after Academician V. Vakhidov, Tashkent, Uzbekistan
Relevance: Kidney transplantation (KT) from a living related donor (LRD) is the only effective alternative treatment for end-stage chronic renal failure (CKD), curing the patient from expensive, long- hours dialysis procedures that adversely affect the general condition of the life. In Uzbekistan, according to the latest data, the incidence of chronic renal failure is approximately more than 700 people per 1 million population
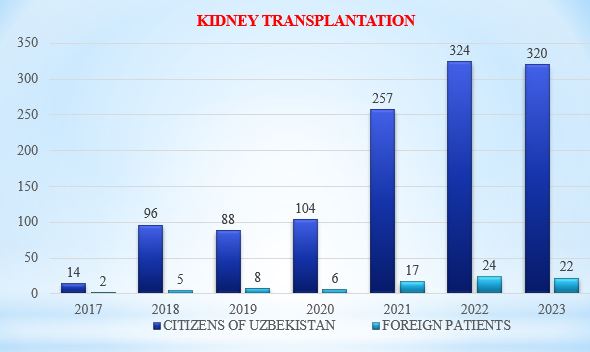
Materials and methods: From 2017 to 2023 in the departments of Vascular Surgery and Kidney Transplantation of the SI "RSSPMCS named after Academician V. Vakhidov", 1250 KT from LRD were performed. This is approximately 82% of the total number of KT, completed during the above period in the Republic of Uzbekistan. Laparoscopic nephrectomy (LN) was performed in 50 cases, and open donor nephrectomy in 1200 cases, since LN started to perform in 2023. After nephrectomy, perfusion of the kidney with a Custodiol solution was immediately started. The time of primary warm ischemia did not exceed 1 minute. To form an arterial anastomosis, the common, less often the external iliac artery was used for an “end to side” anastomosis, and the “end to side” venous anastomosis was formed with the external iliac vein with a transition to the common vein. The duration of cold ischemia is 11 minutes. Duration of secondary warm ischemia 26 min.
The patient was pre-induced with Simulect 20 mg or ATG at a dose of 500-1000 mg. Infusion Methylprednisolone was performed at a dose of 500-1000 mg. Ureterovesical was formed according to the Lich technique, using a ureteral seahorse stent of size 4-5F.
Research results: Complications of the early postoperative period were: urological (urinary tract obstruction) – 17 (1.36%) cases, for 7 of them performed surgical reconstruction, others were cured with endourological treatment methods, acute immunological – 82 (6.56%) cases, infection related complications – 9 (0.72%) cases, lymphocele – 11 (0.88%) cases, death at inpatient period– 7 (0.56%) and 41 death cases where occurred in first 3 years of surgery. Vascular (arterial and venous) complications were not observed. Immunological complications in 75 cases were eliminated after immunosuppressive therapy with various drugs, and plasmapheresis according to KT protocols. In 94% of patients, clinical renal failure disappeared in the early postoperative period. The blood plasma creatinine level (decrease to 120 μmol/L or less) normalized on average by 4.2 days. 1 month after transplantation, this indicator was 0.1 mmol/l, the level of glomerular filtration 5 days after transplantation was 85 ml/min.
Conclusion: The rapid starting of graft function, the rapid resolution of possible rejection crises and postoperative complications is not only compatibility between the related donor and the recipient, but is also largely depended to a reduction in cold ischemia time, thereby reducing the severity of reperfusion injuries.
[1] Kidney transplantation
[2] living related donor
[3] chronic renal failure
[4] renal replacement therapy
