Association between estimated glomerular filtration rates at initiation of dialysis and all-cause mortality in kidney transplant recipients with a failing kidney allograft
Dharshana Sabanayagam1,2,3, Farzaneh Boroumand1,2, Katrina Chau4,5, Eric Au6,7,8, Shuvo Baker1, Ryan Gately9,10, Pedro Lopez11,12,13, Wai Lim11,14, Armando Teixeira-Pinto1,2, Germaine Wong1,2,3.
1Sydney School of Public Health, University of Sydney, Sydney, Australia; 2Centre for Kidney Research, The Children’s Hospital at Westmead, Sydney, Australia; 3Department of Renal and Transplantation Medicine, Westmead Hospital, Sydney, Australia; 4School of Medicine, Western Sydney University, Sydney, Australia; 5Department of Renal Medicine, Blacktown Hospital, Sydney, Australia; 6Australia & New Zealand Dialysis & Transplant Registry, South Australian Health & Medical Research Institute, Adelaide, Australia; 7School of Population and Global Health, University of Melbourne, Victoria, Australia; 8Department of Renal Medicine, The Alfred Hospital, Melbourne, Australia; 9Department of Nephrology, Princess Alexandra Hospital, Queensland, Australia; 10School of Medicine, The University of Queensland, Queensland, Australia; 11Faculty of Health & Medical Sciences, University of Western Australia, Perth, Australia; 12Pleural Medicine Unit, Institute for Respiratory Health, Perth, Australia; 13Grupo de Pesquisa em Exercício para Populações Clínicas (GPCLIN), Universidade de Caxias do Sul, Rio Grande do Sul, Brazil; 14Department of Renal Medicine, Sir Charles Gairdner Hospital, Perth, Australia
Introduction: Graft loss is a devastating outcome for kidney transplant recipients because of the 3-times increased risk of death in patients returning to dialysis compared to those with a functioning transplant (9.4% vs. 2.8%). The effects of estimated glomerular filtration rate (eGFR) thresholds at the time of dialysis initiation in incident dialysis patients on all-cause death have been examined in clinical trials, but not in patients with failing grafts. This study aimed to determine whether the eGFR trajectories post-transplantation and eGFRs at the time of dialysis initiation were associated with survival outcomes post-allograft loss.
Method: Data from the Australian and New Zealand Dialysis and Transplant (ANZDATA) registry was used to identify patients who experienced first kidney allograft loss and commenced dialysis between 2018-2022. The 2021 CKD-EPI creatinine equation was used to calculate eGFR from the recorded serum creatinine measurements. Latent class mixed models (LCMM) were then used to determine eGFR trajectory subclasses post-transplantation until dialysis initiation. We used adjusted Cox proportional hazards models to determine the association between eGFR at the time of dialysis initiation and eGFR trajectory subclasses with all-cause mortality on dialysis.
Results: Within the cohort of 1131 eligible transplant recipients, five distinct classes of eGFR trajectories were identified post-transplantation (Figure 1): class 1 (6.3%), class 2 (63.4%), class 3 (2.4%), class 4 (16.7%), class 5 (11.2%).
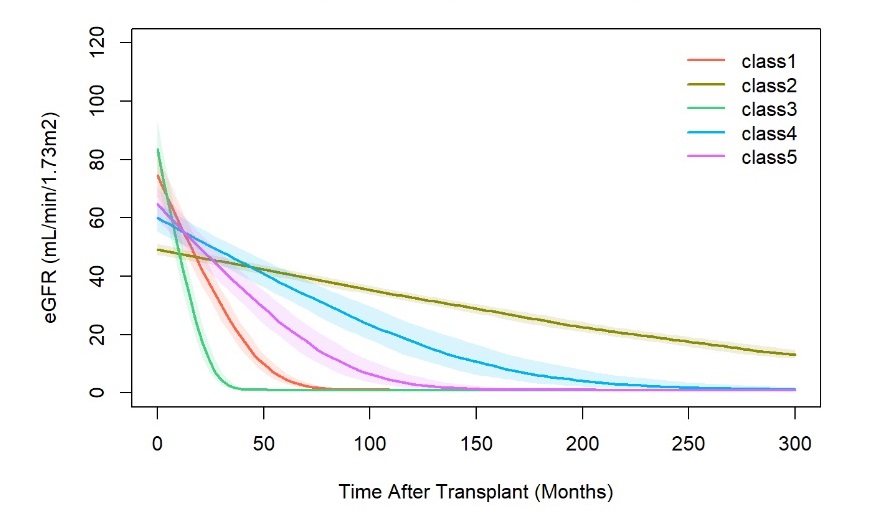
In the adjusted Cox model (HR 95%CI), there were no significant differences in the risk of death post-dialysis initiation between the five classes of eGFR trajectory (Class 1 [reference], Class 2 [1.11, 0.63-1.98, p = 0.717], Class 3 [0.94, 0.27-3.31, p = 0.919], Class 4 [1.22, 0.67-2.23, p = 0.523], Class [1.00, 0.53-1.89, p = 0.996]) or between different levels of eGFR, with HR (95%CI) of 1.02 (0.99-1.05, p= 0.198) per mL/min/1.73m2 increase in eGFR.
Conclusion: Our study did not find any significant differences in survival outcomes post-allograft loss between varying levels of eGFR at dialysis initiation, and between different eGFR trajectories post-transplantation. This suggests that the patterns of eGFR decline since transplantation, and eGFR at the time of dialysis initiation in patients with failing allografts were not associated with long-term patient survival. Consistent with trial-based data observed in incident dialysis patients, eGFR at the time of dialysis commencement in patients who have lost their allografts may not influence long-term patient outcomes.
[1] Allograft Loss
