Outcome of delayed graft function and slow graft function in renal transplant recipients in a tertiary care Centre in eastern India
Sourav Sadhukhan1, Aarpita Raychaudhury1, Atanu Pal1, Sanjay Dasgupta1, Arunanshu Banerjee1.
1Nephrology, IPGMER and SSKM hospital, Kolkata, India
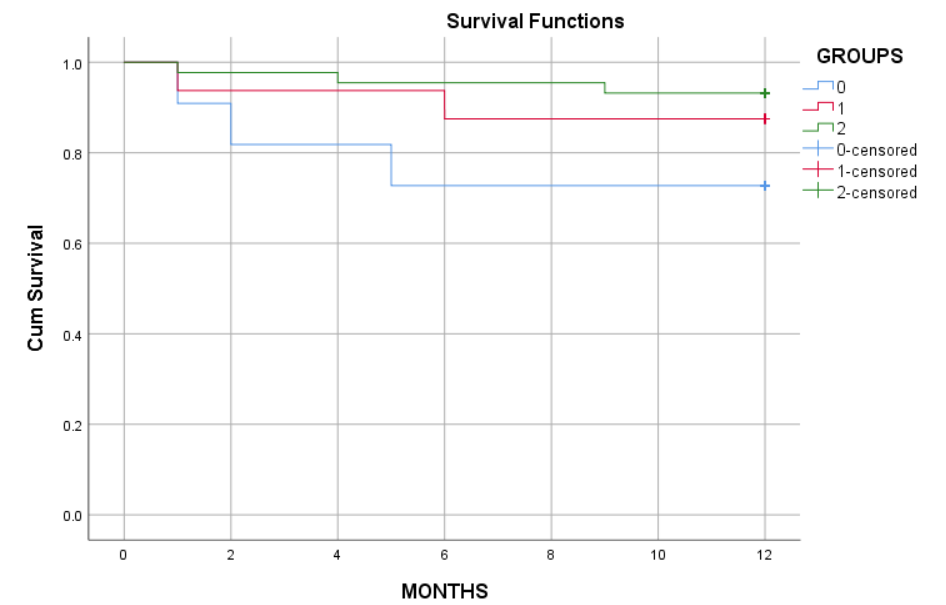
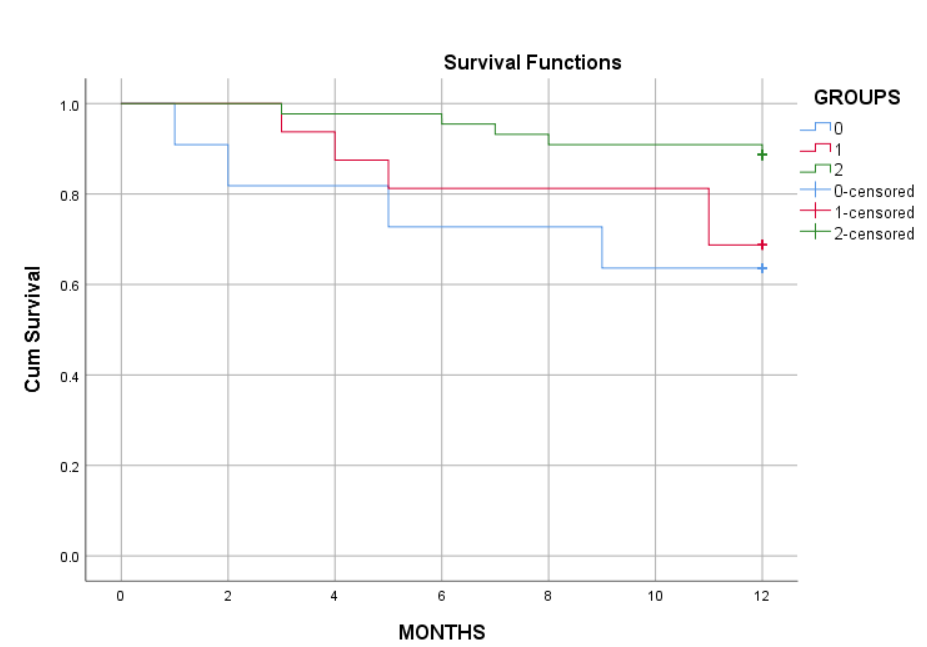
Slow graft function is defined as failure of attainment of an absolute level of Cr by a given postoperative day (POD), Cr ≥3 mg/l on POD5 or Cr ≥2.5 on POD7 or Cr reduction ratio of <30% between POD1 and POD2. Delayed graft function is defined as the need for dialysis during the first week after transplantation. SGF and DGF are cause for decreased allograft survival, and increased mortality. Aims and objectives of our study was to evaluate the incidence of SGF and DGF in our centre and outcome of SGF and DGF when compared with EGF (expected graft outcome). This was a Retrospective cohort analysis, Time period between january 2021 to march 2022 with minimum follow up – 1 year. Total Renal transplant done in this time period was- 71 (live-48, deceased- 23). They were divided intp 3 cohorts – EGF, SGF and DGF. mean age of the patients was 36.7 years, 77.46% patients were male, mean HD vintage was 457 days. out of total 71 renal transplants 61.97% patients had EGF,21.53% patients had SGF and 15.49% patients had DGF. Death censored graft survival at end of 1 year was 88.4% in EGF, 62.4% in DGF (p= 0.002) and 83.7% in SGF (p=0.17). Cumulative patient survival at end of 1 year was 96.7% in EGF, 84.2% in SGF (p=0.37), and 83.4% in DGF group(p=0.004). Rejection free graft survival at end of 1 year was 88.7% in EGF, 64.6% in SGF, 62.3% in DGF. Rejection episodes were more in DGF group (36.4%), p=0.003, than SGF (31.3%), p=0.04, and EGF group (11.36%). In conclusion, Patients with SGF appear to represent an intermediate phenotype. Risk of graft loss and mortality lower than DGF, while almost similar to IGF, but more number of rejections than IGF. Future work should be undertaken to investigate events in the immediate post-transplantation period to improve the prediction of key clinical outcomes. More intensive surveillance of these patients, both with respect to immunosuppressive drug level monitoring and graft structure/function needed.