One year pathological and clinical outcomes of recipients of donor exchange kidneys
Lillian W Gaber1,2, Linda W Moore2,3, Andrea M Meinders3, Adib Edilbi3, Luan Troung1,2, Roberto Barrios1,2, Ziad El-Zaatari1,2, Stephanie G Yi2,3, Richard J Knight2,3, A. Osama Gaber2,3.
1Pathology and Genomic Medicine, Houston Methodist Hospital, Houston, TX, United States; 2Weill Cornell Medicine, New York, NY, United States; 3Surgery, Houston Methodist Hospital, Houston, TX, United States
Introduction: Paired kidney donation (PKD) and donor exchanges provide an opportunity to transplant highly sensitized and blood group incompatible donor-recipient pairs. We sought to examine the first-year biopsy and clinical outcomes of recipients of donor exchange kidneys (PKD) contrasted to recipients receiving direct donation from their biologic (DBD) or non-biologic (DNBD) donor.
Methods: We reviewed 1416 living donor (LD) recipients and compared 288 PKD recipients (Good Samaritan 54, swaps 208, altruistic donor recipient 26) to DBD (623) and DNBD (505) recipients. Frequencies and proportions were used for reporting categorical variables. Continuous variables were reported as means (SD) or medians (IQR). Group comparisons were performed using Chi-square or one-way analysis of variance for parametric data or Kruskal Wallis for non-parametric data.
Results: Of the 1416 LD recipients, 140 had acute rejection (AR; 9.5%) with 31 experiencing antibody-mediated rejection (AMR; 2.2%), for all LD recipients, 1-year eGFR was a median of 60.8 ml/min/m2 (49.4,74.6) & unadjusted patient and graft survival were 98.6% and 96.6%.
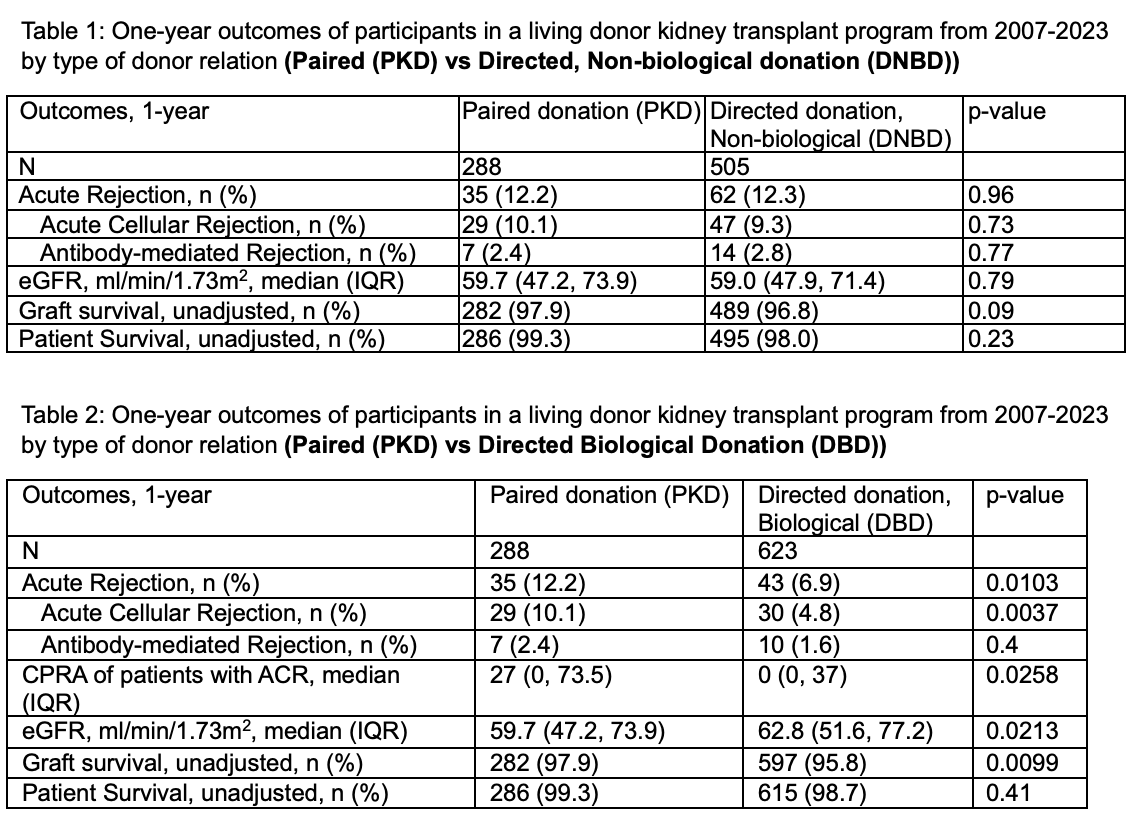
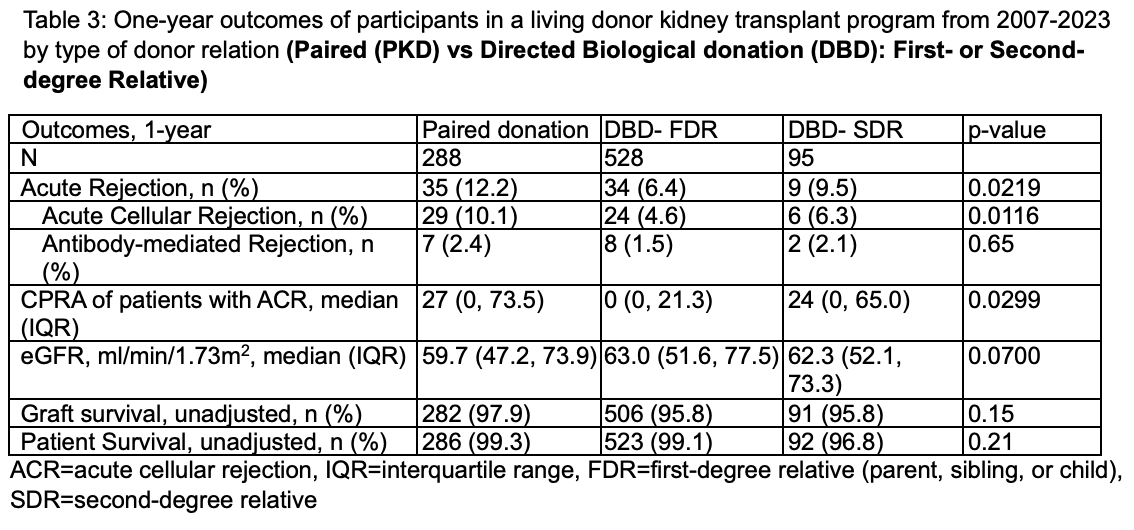
AR rates were similar in PKD recipients vs DNBD (12.2% vs 12.3%) as were other clinical outcomes (Table 1) despite a higher proportion of retransplants and patients with high calculated panel-reactive antibodies (CPRA). AR rates were higher in PKD vs DBD recipients (p<.01) with the difference accounted for by the higher ACR rates (10.3% vs 4.5%; p<0.03). PKD recipients with ACR were more frequently retransplants, had significantly higher CPRA, lower 1-year eGFR (59.7 vs 62.8 cc/min/m2), yet had a higher 1-year graft survival (97.9% vs 95.8%; p<p.05) than DBD recipients (Table 2). DBD Recipients of first-degree relative kidneys (FDR) had the lowest pretransplant CPRA and ACR rates (Table 3).
Conclusion: Our data demonstrate equivalent pathologic and clinical outcomes between PKD recipients and DNBD recipients. DBD recipients have lowest 1st year ACR rates and appear to benefit from lower CPRA and retransplant rates, yet this is not reflected in 1-year survival. PKD offers a transplant opportunity for the hard-to-match patients, and more research into matching, immune monitoring and immune-suppression is needed to reduce AR rates.
Andrea M Meinders is a Burroughs Wellcome Fund Fellow supported by a Burroughs Wellcome Fund Physician Scientist Institutional Award to the Texas A&M University Academy of Physician Scientists.
[1] Living donor kidney transplantation
[2] Paired donation
