
Multivariable prognostic factors in a large multicenter cohort of post-transplantl disorders (PTLD): WHO classification and type of organ transplant impact the event-free survival
Vikas Dharnidharka1, Lujain Jaza1, Mansi Agarwal1, Charles W Goss, for the PTLD-MSMS group1.
1Washington University School of Medicine, St. Louis, MO, United States
PTLD-MSMS.
Background: PTLDs are a relatively rare but devastating complication of solid organ and hematopoietic tissue transplant, often driven by Epstein-Barr virus (EBV). Prior published series noted different and conflicting variables that affected patient survival.
Methods: As part of our National Institutes of Health funded multicenter study, we have collected from 3 large USA transplant centers a large cohort of paraffin embedded PTLD tissues for metagenomic viral sequencing, along with highly granular clinical data. In this analysis, we used the extensive clinical data to fit a multivariable time to event model for 5-year composite event-free survival after a PTLD diagnosis and calculate adjusted hazard ratios (AHR) for covariates. Events were defined as repeat PTLD, allograft failure or patient death, censored at first event.
Results: Our full USA cohort has accumulated 366 PTLD tissues from 1991-2022 from 313 unique patients. This analysis focuses on 230 patients for whom we have the tissue of their first PTLD event and data on rituximab, excluding those where the tissue is only from a subsequent PTLD event. Cohort characteristics included: median age 23.4 years, male 59%, Caucasian 77%, late PTLDs > 1 year after transplant 155 (67%). Organ transplant type was kidney (22%), heart (24%), lung (22%), liver (15%) and others (17%). The 2 most common PTLD locations were lymph node (53%) and GI tract (33%). 118 (52%) developed one of the composite events. Of the 230 tissues, 143 (62%) were EBV positive. By the 2016 WHO classification, tissues were classified as non-destructive (13; 5.7%)., polymorphic (38; 17%), Burkitt (10; 4.3%), T cell (9; 3.9%), other monomorphic (145; 63%), or Hodgkin (15; 7%). Rituximab was given in 167 and chemotherapy in 136.
In Kaplan-Meier univariable analyses, the destructive WHO types showed worse survival compared to non-destructive (Figure).
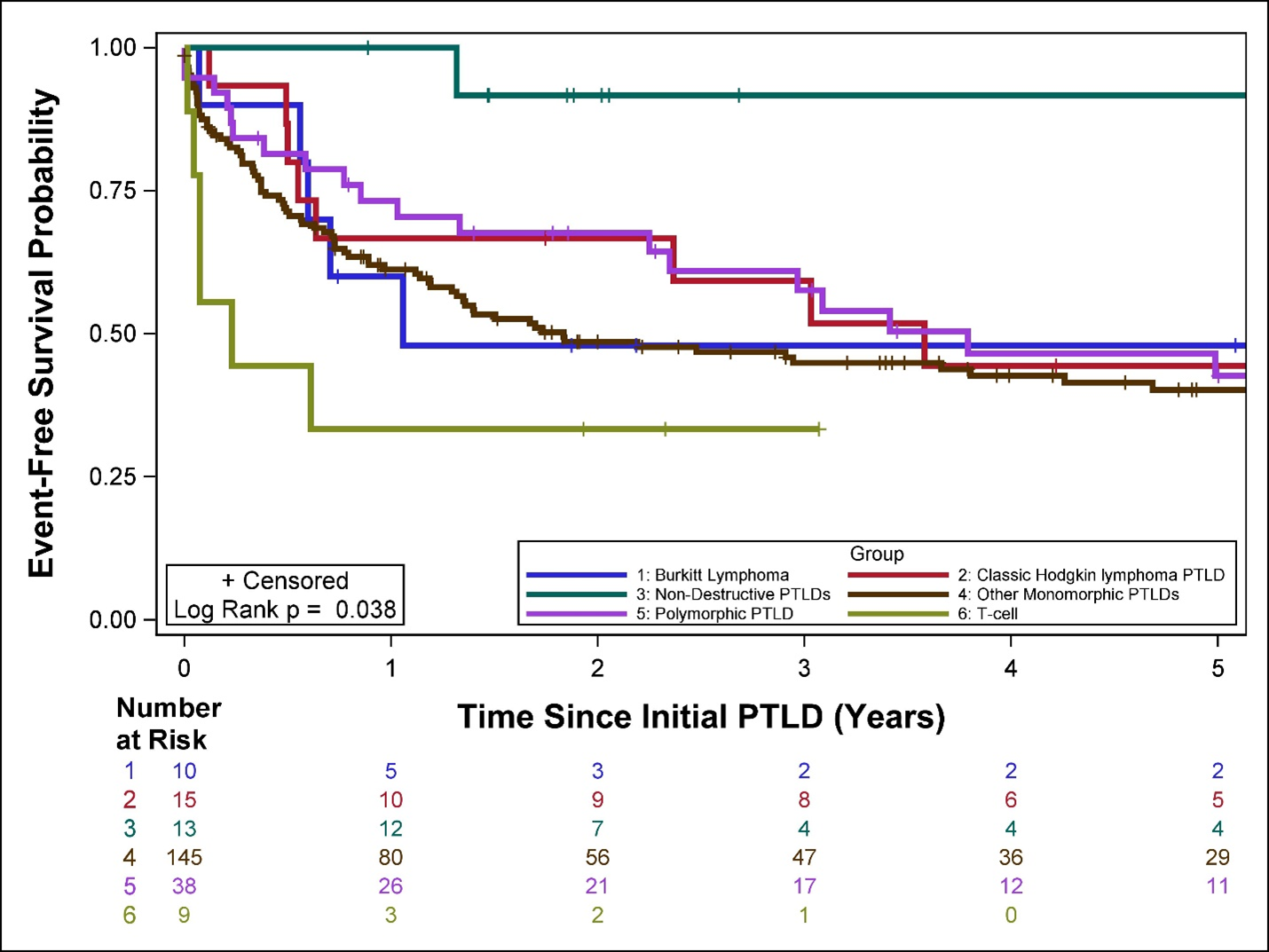
In a multivariable model, organ transplant types (lung AHR 1.91, hematopoietic AHR 2.36; both p = 0.04;) and WHO classification types Burkitt’s (AHR 11.04; p = 0.03), T cell PTLD (AHR 17.04; p = 0.03); and other monomorphic (AHR 9.43; p = 0.03,) were significantly associated with worse event-free survival, while liver organ transplant type was protective (AHR 0.39; p = 0.03). No other clinical covariates were significant.
Conclusions: In this large multicenter series, 5-year event-free survival was impacted adversely by certain WHO types and by certain organ transplant types, even after adjustment for multiple clinical covariates.
This work has been supported by grant R01AI142135 to Dr. Vikas Dharnidharka, from the National Institute of Allergy, Immunology and Infectious Diseases branch of the National Institutes of Health, USA..
[1] post-transplant lymphoproliferative disorders, Epstein-Barr virus infection, lymphoma, complication of immunosuppression, event-free survival
