Utilizing large language models for predictive analysis of intraoperative hemorrhage risks in lung transplant recipients
Bingqing Yue1,3, Yang Yan2,3, Juan Chen1,3, Man Huang1,3, Jingyu Chen1,3.
1Department of lung transplantation, The Second Affiliated Hospital Zhejiang University School of Medicine, Hangzhou, People's Republic of China; 2School of Engineering, Westlake University, Hangzhou, People's Republic of China; 3Zhejiang University, Hangzhou, People's Republic of China
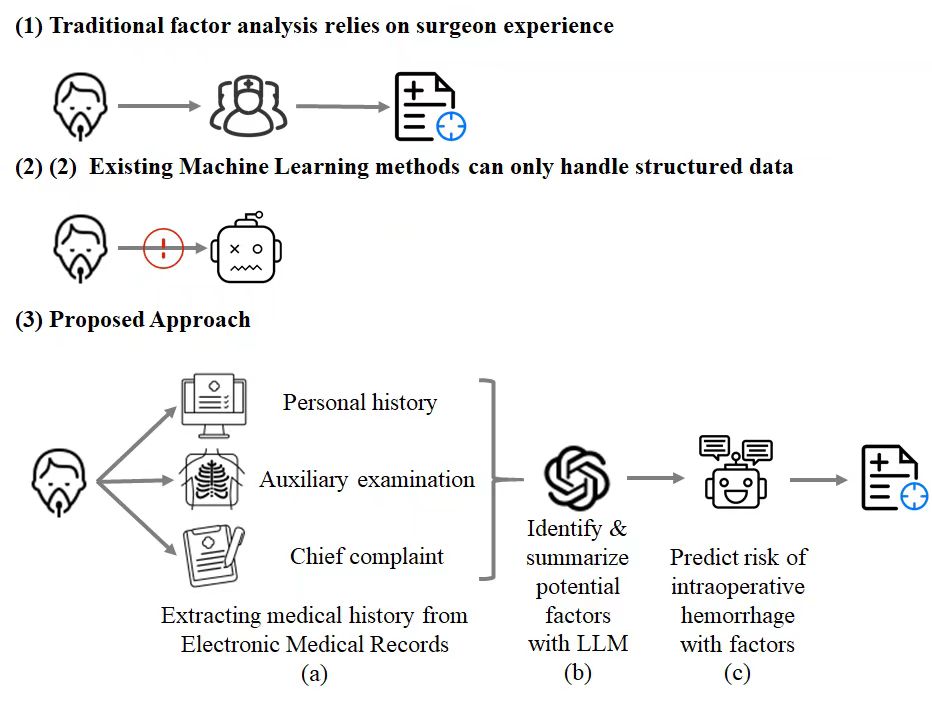
Introduction: Intraoperative hemorrhage remains one of the most formidable complications in lung transplantation, significantly elevating mortality rates. Current identification of risk factors, such as specific lung diseases, the employment of Extracorporeal Membrane Oxygenation (ECMO), and surgical approaches, is predominantly experiential, relying heavily on surgeons' subjective judgments. This method not only lacks efficiency but also precision, especially given the vast and complex data available in the medical histories of lung transplant recipients. The challenge lies in systematically identifying potential risk factors and accurately predicting intraoperative hemorrhage risks.
Method: We introduce an innovative approach that leverages a Large Language Model (LLM) to sift through the medical histories of lung transplant recipients and identify those at high risk of intraoperative hemorrhage. By extracting comprehensive medical data from Electronic Medical Records (EMR) and analyzing it through an LLM trained on extensive medical literature and clinical notes, our method discerns intricate correlations between patients' histories and hemorrhage risks. The LLM predicts hemorrhage probabilities, allowing for the categorization of potential risk factors. Subsequently, these categorized factors serve as the foundation for developing a predictive machine learning model.
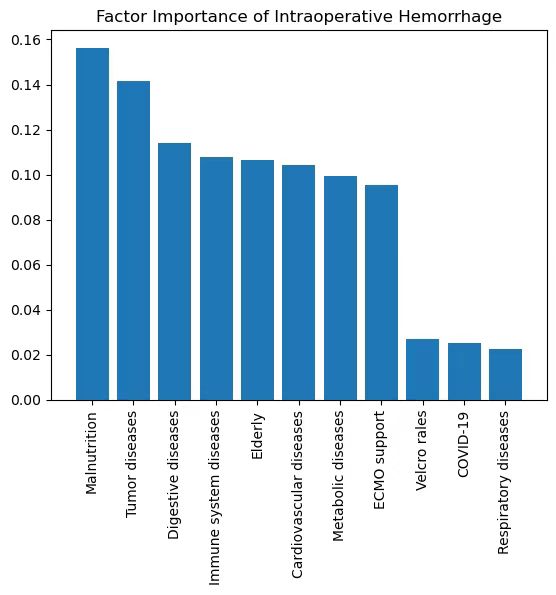
Results: Our retrospective study of 41 lung transplant recipients demonstrates the efficacy of this method, achieving an Area Under the Curve (AUC) of 0.9375. By inputting detailed medical histories into the LLM, we identified 211 potential risk factors, which were then grouped into 11 categories, including but not limited to Respiratory Diseases, Cardiovascular Diseases, ECMO Support, and COVID-19. Utilizing these factors, a Random Forest model was trained, resulting in the aforementioned AUC, signifying high accuracy in predicting intraoperative hemorrhage risks.
Conclusion: This study marks the inaugural application of an LLM in forecasting intraoperative hemorrhage risks in lung transplant recipients. Our methodology not only surpasses traditional, surgeon-based assessments in identifying potential risk factors but also excels in predicting the likelihood of hemorrhage with notable precision. The insights gained here can significantly aid surgeons in decision-making, thereby enhancing lung transplantation outcomes. Future endeavors will focus on validating this approach with a more extensive dataset and investigating its applicability to other transplantation complications.
We thank Google for offering Google Cloud Platform credits.
[1] Hemorrhage
[2] Data Mining
[3] Large Language Model
[4] Lung Transplantation
